Autumn Weather and Winter Increase in Cerebrovascular Disease Mortality
R McDonagh, J Harbison
Mercer’s Institute, St James’s Hospital, James’s St, Dublin 8
Abstract
Mortality from cerebrovascular disease increases in winter but the cause is unclear. Ireland’s oceanic climate means that it infrequently experiences extremes of weather. We examined how weather patterns relate to stroke mortality in Ireland. Seasonal data for Sunshine (% of average), Rainfall (% of average) and Temperature (degrees Celsius above average) were collected for autumn (September-November) and winter (December-February) using official Irish Meteorological Office data. National cerebrovascular mortality data was obtained from Quarterly Vital Statistics. Excess winter deaths were calculated by subtracting (nadir) 3rd quarter mortality data from subsequent 1st quarter data. Data for 12 years were analysed, 2002-2014. Mean winter mortality excess was 24.7%. Winter mortality correlated with temperature (r=.60, p=0.04). Rise in winter mortality correlated strongly with the weather in the preceding autumn (Rainfall: r=-0.19 p=0.53, Temperature: r=-0.60, p=0.03, Sunshine, r=0.58, p=0.04). Winter cerebrovascular disease mortality appears higher following cool, sunny autumns.
Introduction
It has recognized for many centuries that there is a seasonal variation in stroke incidence and mortality with an increase in incidence of deaths in the winter months. The first publication to use the word ‘stroke’ in describing apoplexy was William Cole’s 1689 work ‘A Physico-Medical Essay Concerning the Late Frequencies of Apoplexies’1 which attributed the increased rate of apoplexy in the winter of 1682 in London to the cold weather of that year. More recently there have been a number of other studies looking at seasonal variation in incidence of stroke and stroke subtypes and association with weather, pollution and other climactic factors2-4. Ireland has a temperate, oceanic weather pattern of mild, wet winters and summers moderated greatly by the effect of the North Atlantic current. In the last 10 years, however, there have been a number of extreme weather events. We examined whether there was any association between the weather experienced in Ireland and quarterly mortality data for cerebrovascular disease.
Methods
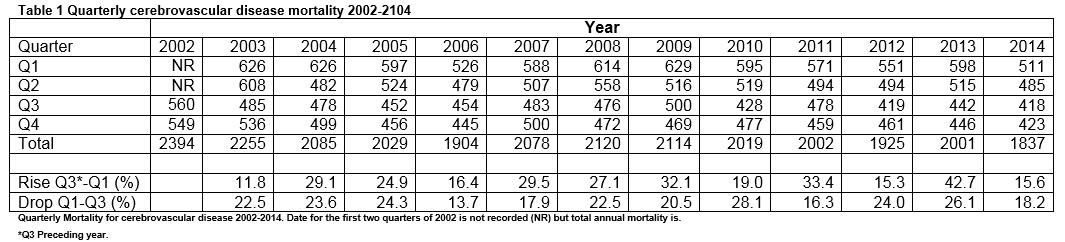
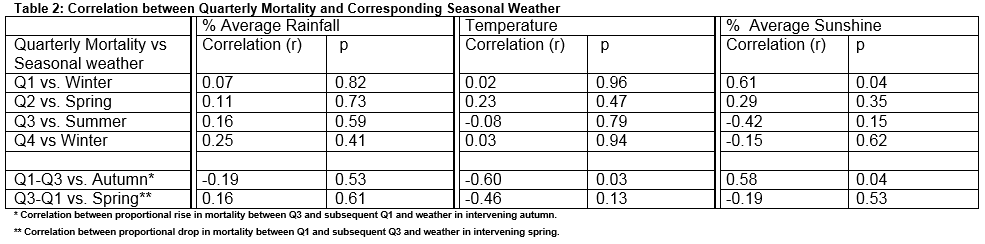
Mortality data for cerebrovascular disease was obtained from Vital Statistics published by the Irish Central Statistics Office (CSO). Although data for stroke mortality has been published since 1864, quarterly data has only been made available since summer 2002. These are divided in to Quarter 1 (Q1: January to March), Quarter 2 (Q2: April to June), Quarter 3 (Q3: July-September) and Quarter 4 (Q4: October to December). Data for weather was obtained from official seasonal reports of the Irish Meteorological Office. Data from the meteorological station nearest to the largest population centre, Baldonnell Aerodrome Dublin, was used for comparison. Data on weather is published seasonally; winter (December to February), spring (March to May), summer (June-August) and autumn (September to November). Data on rainfall (% long term average), sunshine (% of long term average hours) and temperature (degrees Celsius deviation from long term average values) were examined. As there has been a gradual improvement in stroke care and outcome during this period, which we felt, might give a false correlation with climactic changes, we also calculated proportional changes between summer (Q3) nadirs and subsequent winter (Q1) peaks in mortality and between winter peaks and subsequent summer nadirs. Data were analysed using Microsoft Excel and SPSS 14.0 to determine the annual changes in cerebrovascular disease mortality between quarters and proportional changes between nadirs of incidence in Q3 and peaks in preceding and subsequent Q1.
Results
CSO attributed 25,478 deaths to cerebrovascular disease in the 12 years between 2003 and 2014. Of these 7032 (27.6%) occurred in Q1 and 6073 (23.8%) in Q3. The median annual proportional rise in cerebrovascular disease between Q3 and a subsequent Q1 was 26.0% (range 15.3% to 42.7%), mean 24.7%. Overall, annual cerebrovascular mortality has decreased by 13.2% over the study period 2003-2014. There is a significant direct correlation between Q1 mortality and winter sunshine (r=.61, p=0.04). No other significant correlations between weather data and cerebrovascular disease mortality in corresponding quarters were found (table 2). There was however a significant correlation between autumn weather and the increase in cerebrovascular disease mortality in winter above the preceding summer. Cooler autumns with more sunshine were associated with a higher proportional rise in subsequent winter cerebrovascular disease mortality. (Deviation from average Temperature: r=-0.60 p=0.03. % Average sunshine: r=0.58, p=0.04. % Average rainfall: r= -0.13, p=0.7). There was no significant correlation between spring weather conditions and proportional drop in cerebrovascular mortality in the subsequent Q3. (Deviation from average Temperature: r=-0.46, p=0.13. % Average sunshine: r=-0.19, p=0.53. % Average rainfall: r= 0.16, p=0.62).
Discussion
Whilst a number of studies have shown various associations between seasonal weather and stroke and cerebrovascular disease2-4, this is the first to show an association between seasonal weather and a subsequent increase in stroke mortality in a future time period.
The study has limitations. Whilst published data for annual mortality in Ireland, including stroke, is available for 150 years, quarterly cerebrovascular disease mortality has only been published since 2002 and is dependent on death certification data, reliability of which is variable in cases of stroke5,6. Although correlations found are reasonably strong and significant it would be interesting to see if the association found continues in subsequent years. Periods of recording of cerebrovascular disease and weather data do not match exactly, with the weather data window preceding that of mortality by one month. However, incident stroke can take several days or weeks to lead to death in affected individuals. Local data reports a median onset to death duration for stroke of 20 days7. Therefore this overlap may in fact better represent incidence of subsequently fatal stroke better than a complete concordance of time intervals, which would miss the lag between stroke onset and death.
The reason for the summer-winter discrepancy in stroke incidence remains unclear. Whilst there is a similar zenith in cardiovascular mortality during winter the annual nadir for deaths from ischaemic heart disease in Ireland occurs later than for cerebrovascular disease in Q4 rather than Q3. Consequently an identical analysis could not be effectively performed for ischaemic heart disease. The findings that winter stroke is more common after cooler but sunnier autumns and in sunnier winters may seem counter intuitive but it could be of consequence that hours of sunshine may reflect reduced cloud cover and thus cooler night-times and frosts in the late autumn and winter. Such apparently transient changes in temperature have been associated with increased risk of stroke both during summer and winter8,9.
Proposed potential reasons for a winter increase in mortality include seasonal variation in atrial fibrillation incidence10, alterations in platelet function and clotting factors11 or reduced physical activity12. Recent work has however shown that epigenetic factors may be relevant with alterations in seasonal expression of some genes13. Although the reason for the winter excess in cerebrovascular disease is still unclear, our findings that climate in the months preceding, influences this mortality may help in the search for a reason behind this phenomenon.
Correspondence: J Harbison
Mercer’s Institute, St James’s Hospital, James’s St, Dublin 8
Email: [email protected]
References
1. Cole W. A Physico-Medical Essay Concerning the Late Frequency of Apoplexies Together With a General Method of Their Prevention and Cure: In a Letter to a Physician. Oxford, United Kingdom; The Theatre; 1689.
2. Palm F, Dos Santos M, Urbanek C, Greulich M, Zimmer K, Safer A, Grau AJ, Becher H. Stroke seasonality associations with subtype, etiology and laboratory results in the Ludwigshafen Stroke Study (LuSSt). Eur J Epidemiol. 2013; 28: 373-381.
3. Díaz A, Gerschcovich ER, Díaz AA, Antía F, Gonorazky S. Seasonal variation and trends in stroke hospitalizations and mortality in a South American community hospital. J Stroke Cerebrovasc Dis. 2013; 22: e66-9.
4.Han MH, Yi HJ, Kim YS, Kim YS. Effect of seasonal and monthly variation in weather and air pollution factors on stroke incidence in Seoul, Korea. Stroke. 2015; 46: 927-935.
5. Corwin LI, Wolf PA, Kannel WB, McNamara PM. Accuracy of Death Certification of Stroke: The Framingham Study. Stroke 1982; 13: 818-821.
6. Sinha S1, Myint PK, Luben RN, Khaw KT. Accuracy of death certification and hospital record linkage for identification of incident stroke. BMC Med Res Methodol. 2008; 8: 74.
7. Ntlholang O, Walsh S, Bradley D, Harbison J. Identifying palliative care issues in inpatients dying following stroke. Ir J Med Sci 2015; Apr8: e published
8. Mostofsky E, Wilker EH, Schwartz J, Zanobetti A, Gold DR, Wellenius GA, Mittleman MA. Short-term changes in ambient temperature and risk of ischemic stroke. Cerebrovasc Dis Extra. 2014; 4: 9-18.
9. Wang Q, Gao C, Wang H, Lang L, Yue T, Lin H. Ischemic stroke hospital admission associated with ambient temperature in Jinan, China. PLoS One. 2013 ;8: e80381
10. Pant S, Badheka AO, Deshmukh A. Higher frequency of atrial fibrillation linked to colder seasons and air temperature on the day of ischemic stroke onset. J Stroke Cerebrovasc Dis. 2013;22: 896.
11. Crawford VL, McNerlan SE, Stout RW. Seasonal changes in platelets, fibrinogen and factor VII in elderly people. Age Ageing. 2003;32: 661-665.
12. McDonnell MN, Esterman AJ, Williams RS, Walker J, Mackintosh SF. Physical activity habits and preferences in the month prior to a first-ever stroke. PeerJ. 2014; 2 e489.
13. Dopico XC, Evangelou M, Ferreira RC, Guo H, Pekalski ML, Smyth DJ, Cooper N, Burren OS, Fulford AJ Hennig BJ, Prentice AM, Ziegler AG, Bonifacio E, Wallace C, Todd JA. Widespread seasonal gene expression reveals annual differences in human immunity and physiology. Nat Commun. 2015; 6: 7000.
P479