Bacteraemia in the ED: Are We Meeting Targets?
N Borhan1, F Borhan2, C Ni Cheallaigh3, B Dinesh4, K O’Reilly5, A Moughty1.
1Emergency Department, Mater Misericordiae University Hospital, Dublin 7, Ireland.
2Emergency Department, Connolly Hospital, Blanchardstown, Dublin 15, Ireland.
3Department of Infectious Diseases, Mater Misericordiae University Hospital, Dublin 7, Ireland.
4Microbiology Department, Mater Misericordiae University Hospital, Dublin 7, Ireland.
5Department of Respiratory Medicine, Mater Misericordiae University Hospital, Dublin 7, Ireland.
Abstract
Aim
An audit was performed in an Irish Emergency department (ED) to evaluate adherence to established antimicrobial guidelines and to determine the most common presentations of sepsis.
Method
Data on ED patients with clinically significant bacteraemia on blood cultures were recorded for three months . The antimicrobial given to the patient was compared to that which the hospital guidelines would recommend for the ED diagnosis.
Result
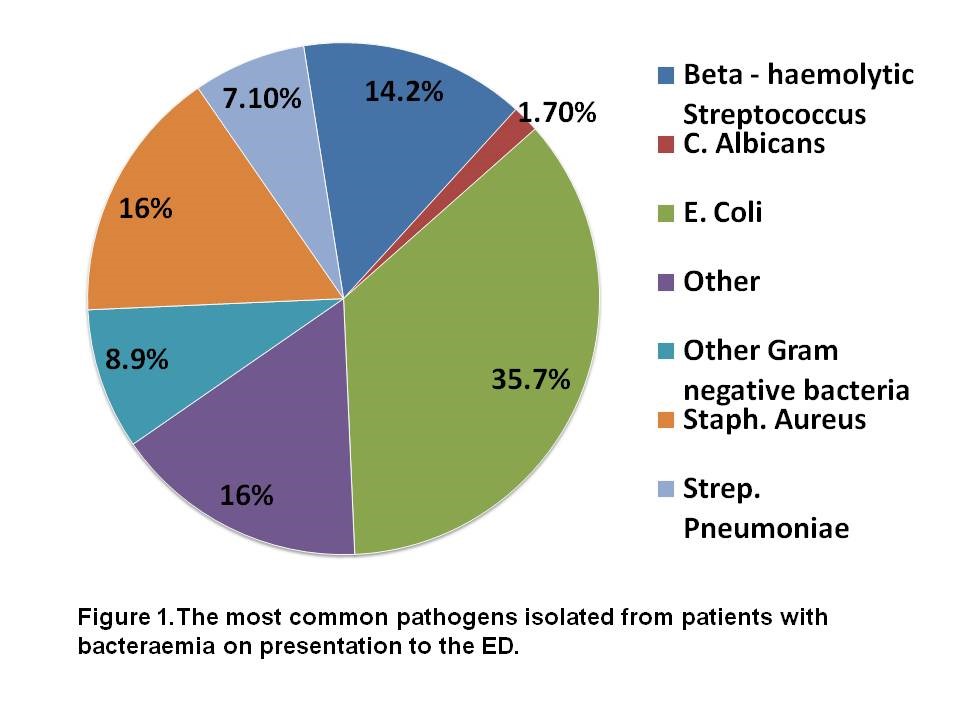
Eleven patients out of 53 had no antimicrobial guidelines for diagnosis. Of the 42/53 patients, non-adherence to antimicrobial guidelines by physicians was observed in 81% (n=34/42) patients and adherence was observed in 19% (n=8/42) patients. Escherichia coli 35.70% (n=18), was the most frequent organism isolated.
Conclusion
Non-adherence to antimicrobial guidelines resulted in 68% (n=23/34) of organisms covered by the antibiotic. Adherence to antimicrobial guidelines resulted in 87% (n=7/8) of organisms covered by the antibiotic.
Introduction
When sepsis is identified early in the Emergency Department (ED) and its severe form is treated aggressively with the protocolised care bundle of early goal directed therapy (EGDT), improvements in mortality are significant1,2. Surviving sepsis guidelines recommend the administration of effective intravenous antimicrobials within the first hour of recognition of septic shock and severe sepsis without septic shock3. The Mater University Hospital has antimicrobial guidelines to guide empiric prescribing in adult sepsis available on the hospital intranet and on a smartphone app.
Methods
A retrospective audit was performed in the Emergency Department of Mater Misericordiae University Hospital, Dublin 7, Ireland. We identified patients with clinically significant bacteraemia on blood cultures taken in the ED between September and November 2014. We determined the time of triage, time seen by ED doctor, time and choice of antimicrobial agent and initial ED diagnosis from the clinical records. The antimicrobial given to the patient was compared to that which the hospital guidelines would recommend for the ED diagnosis. Descriptive statistics were generated using SPSS.
Results
There were 119 patients with positive results on blood cultures taken in the ED between September and November 2014, identified from a database maintained by the Microbiology Department. Blood cultures growing coagulase-negative Staphylococci, Gram-positive bacillii or Propionibacter in the absence of a history suggestive of infection with these organisms (n=66) were classified as probable contaminated and excluded from further analysis. Our study included 53 patients, 31 males and 22 females. The median age of patients in our study was 63 years (21 to 92 years). The median time from triage to a sepsis patient seeing an ED physician was 26 minutes. Thirty eight out of 53 patients (71.6%) had a serum lactate measured. Forty-three out of 53 patients (81.1%) received antibiotics, 22 of which received antibiotics after one hour. The median time to administration of antibiotics was one hour and 15 minutes. Forty out of 53 patients (75.4%) received intravenous fluid resuscitation, 17 of which got intravenous fluids after one hour. The median time from seeing an ED doctor to commencing intravenous fluids was 46 minutes.
Pneumonia, Urosepsis and sepsis of unknown origin are the most common diagnoses in bacteraemic individuals in the Emergency Department. The most frequent organisms isolated from bacteraemic individuals in the ED were Escherichia Coli 35.70% (n=18), Staphylococcus Aureus 16% (n=10), Beta-haemolytic Streptococci 14.20% (n=8) and Streptococcus Pneumoniae 7.10% (n=4) ,Figure 1. Escherichia coli is the most common pathogen isolated from patients with bacteraemia on presentation to the ED. Of the 18 isolates of E. coli,10 were resistant to Co-amoxiclav, 5 were resistant to Ciprofloxacin and two were resistant to Gentamicin. Two out of 8 Beta-Haemolytic Streptococci were resistant to Penicillin. None of the 10 isolates of Staphlyococcus Aureus were resistant to Flucloxacillin. The antimicrobial prescribed by the ED doctor was compared to that recommended by the Hospital antimicrobial guidelines for the initial diagnosis. The sensitivity of the organism to the antimicrobial initially prescribed was determined from the microbiology database.
There were no antimicrobial guidelines for diagnosis in 11/53 patients. Of the 42/53 patients, non-adherence to antimicrobial guidelines by physicians was observed in 81% (n=34/42) patients and adherence was observed in 19% (n=8/42) patients.
Non-adherence to antimicrobial guidelines resulted in 68% (n=23/34) of organisms covered by the antibiotic, while 32% (n=11/34) were not. Adherence to antimicrobial guidelines resulted in 87% (n=7/8) of organisms covered by the antibiotic, while 13% (n=1/8) were not. During the hospital admission 5/53 individuals died. In all 5 individuals, the empiric antibiotic chosen in the ED covered the pathogen isolated from their bloodstream.
Discussion
Pneumonia, Urosepsis and sepsis of unknown origin are the most common ED diagnoses in individuals with significant bacteraemia on presentation to the ED. E. coli is the most common pathogen isolated from patients with bacteraemia on presentation to the ED. Adherence to antimicrobial guidelines is poor. Failure to cover the organism subsequently isolated from the bloodstream is more common with non-adherence to antimicrobial guidelines. Targets of administration of intravenous fluids and antibiotics within 1 hour are frequently missed. Adherence to such hospital guidelines is often low to moderate (40%–60%)4,5 . Further efforts are needed to explore reasons for non-adherence to antimicrobial prescribing guidelines.
Conflict of interest
The authors declare that they have no conflict of interest.
Correspondence:
Dr.Nafisah Borhan, Clinical Lecturer in Department of Emergency Medicine at the Royal College of Surgeons in Ireland.
Email: [email protected]
References
1.Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M; Early Goal-Directed Therapy Collaborative Group. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001 Nov 8;345(19):1368-77.
2. Osborn T, Nguyen B, Rivers EP. Emergency Medicine and the Surviving Sepsis Campaign: An International Approach to Managing Severe Sepsis and Septic Shock. Ann Emerg Med. 2005;46:228–231.
3. National Clinical Effectiveness Committee (NCEC). Sepsis Management. National Clinical Guideline No. 6, November 2014 [cited 2015 July 27]. Available from: http://www.hse.ie/eng/about/Who/clinical/natclinprog/sepsis/sepsis%20management.pdf
4.Halm EA, Atlas SJ, Borowsky LH, Benzer TI, Metlay JP, Chang YC, et al. Understanding physician adherence with a pneumonia practice guideline: effects of patient, system, and physician factors. Arch Intern Med. 2000;160:98–104
5. van de Beek D, de Gans J, Spanjaard L, Vermeulen M, Dankert J Antibiotic guidelines and antibiotic use in adult bacterial meningitis in The Netherlands. J Antimicrob Chemother. 2002;49:661–6
(P720)
