Bilateral Neonatal Suppurative Sialadenitis Progressing to Abscess Formation in a Preterm Neonate
N. Shaughnessy1, T. McGrath2, M. Moore2, B.H. Walsh1
1. Department of Neonatology, Cork University Maternity Hospital, Wilton, Cork, Co. Cork, Ireland
2. Department of Radiology, Cork University Hospital, Co. Cork, Ireland
Abstract
Aims
We report a case of bilateral neonatal suppurative sialadenitis (NSS) in an extremely low birth weight infant (ELBW).
Methods
The infant developed bilateral sub-mandibular swelling at 3 weeks of age. NSS with abscess was confirmed with ultrasound. Despite intravenous antibiotic therapy the masses increased in size and developed abscesses.
Results
Unilaterally the abscess discharged via Wharton’s duct necessitating intubation to protect the airway. The abscess remnant was incised and drained. Culture grew a methicillin sensitive staphyloccocus aureus. The NSS resolved following two weeks of antibiotics.
Conclusion
We wish to highlight the importance of early recognition of this rare condition in preterm neonates.
Introduction
Suppurative sialadenitis is an infection of the salivary glands. Its occurrence in the neonatal population is extremely rare, however the exact incidence is unclear with the literature being limited to a small number of cases reports and cases series. Despite being uncommon it can have significant clinical implications, including disseminated sepsis, osteomyelitis and airway compromise. Therefore the clinician should consider this possible differential when reviewing a neck swelling in the newborn.
We present the case of a premature female infant who developed a bilateral submandibular suppurative sialadenitis, and discusses the aetiology, complications and management of NSS.
Case Report
A preterm female infant was born at 27+3 weeks gestation (580g) following an emergency Caesarean Section for intrauterine growth restriction, with reversed end diastolic flow.
At delivery she was intubated and ventilated due to respiratory distress syndrome. She was extubated to non-invasive ventilation on day of life 5, but required re-intubation on day 10 for apnea. She was screened for infection at that time with a full blood count, CRP and blood culture and received 5 days of antibiotics, but cultures remained negative. By day 14 she had been extubated again to nasal continuous positive airway pressure and had achieved full enteral nutrition.
On day of life 18, bilateral submandibular masses were noted on routine physical examination. Theses increased in size over a few hours. They were large, firm and erythematous. The remainder of her examination was unremarkable, including normal vital signs.
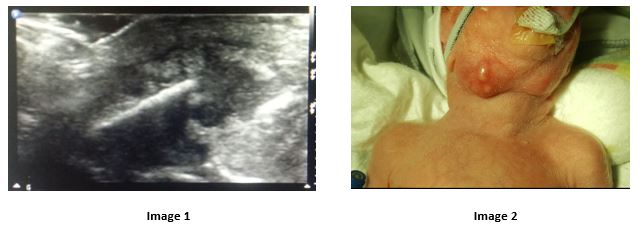
The primary differential included a developing abscess, with lymphadenitis a less likely alternative. A partial septic work-up was performed including full blood count, CRP and blood culture and she was commenced on empirical intravenous antimicrobials (teicoplanin, gentamicin and flucloxacillin). An ultrasound scan demonstrated bilateral hypoechoic soft tissue masses in the submandibular region, consistent with bilateral submandibular sialadenitis (see image 1). Following this, and in discussion with microbiology, antimicrobial treatment was rationalised to intravenous co-amoxiclav (for additional aerobic cover) and gentamicin.
Over the following days, the neck masses progressively increased in size. They were more erythematous and firm with new puncta present (see image 2). On day of life 21, she had an acute apnoeic event and a large volume of purulent serosanguinous fluid was suctioned from the oropharynx. There was no sign of abscess in the floor of the mouth and this likely had discharged from the Wharton’s duct. Following initial stabilization, she was intubated to ensure the airway was protected and the external abscess was incised with a 25 gauge needle and allowed to drain. She remained intubated for five days and completed 13 days of intravenous co-amoxiclav. This wound healed by secondary intention.
Discussion
Suppurative sialadenitis is an uncommon infection in newborn infants. Typically, it involves the parotid gland1, with the submandibular gland being a rarer site of primary infection2,3. In fact, a review specifically of submandibular NSS, found a total of only 39 cases reported in the medical literature to-date.4 NSS was unilateral in 84% (33/39) 4 of cases. Identified risk factors include prematurity, orogastric feeding, dehydration and supported ventilation1, 3, 4, 7. The clinical presentation is typically an erythematous, tender, submandibular mass in the absence of systemic signs5. While NSS is primarily a clinical diagnosis, the use of ultrasound can aid in the diagnosis3 (Image 1), the differential for which includes: venous malformations, haemangiomas, lymphadenitis or congenital tumours.8
The most common causative organism is Staphylococcus aureus. The standard first line of treatment includes airway monitoring and management if required, and empiric intravenous antibiotics. Once cultures have determined the organism and sensitivities, the antibiotic therapy should be adjusted accordingly.
There is limited evidence available to guide treatment in the ELBW population. In cases that fail to respond to appropriate intravenous antibiotics, alternatives that have been proposed include incision and drainage5, or manual compression and expression of pus from Wharton’s duct7. Both of these may be technically challenging in a small ELBW infant and neither is without risk. Incision and drainage has been associated with adverse events such as facial nerve weakness, lingual or hypoglossal nerve damage, haemorrhage and sinus formation6. Contrary to this the risks associated with manual compression include abscess rupture, septicaemia and aspiration resulting in respiratory compromise7. Therefore, neither option should be under-taken lightly but rather should be considered dependent upon the clinical necessity and when possible with subspecialist support.
The case discussed highlights the importance of early recognition of NSS. It has the potential to cause significant life threatening events, in particular airway obstruction upon rupture of the abscess. To the best of our knowledge, this is the first case of NSS reported in an ELBW infant in Ireland.
Consent
Consent has been obtained from the patient’s primary caregiver to discuss the patients hospital course as above.
Conflicts of Interest Interest
The authors do not have a conflict of interest with the issues raised in this paper.
Funding Statement
No funds external to our department were sought or obtained for the preparation of this paper.
Corresponding Author
Dr. Niamh Shaughnessy,
Cork University Maternity Hospital,
Co. Cork,
Ireland.
Email: [email protected]
References
1.) D. Leake, R. Leake, Neonatal suppurative parotitis, Paediatrics 46 (1970) 203-207
2.) D.H. Wells, Suppuration of the submandibular salivary glands in the neonate, Am. J. Dis. Child. 129 (1975) 628- 630.
3.) W.W. Banks, S.D. Handler, G.B. Glade, H.D. Turner, Neonatal submandibular sialadenitis, Am. J. Otolaryngol. 1 (1980) 261- 263
4.) M.D. Alvarez, B.A. Batista, L.R. Ales, Neonatal acute suppurative submandibular sialadenitis. Literature reports from 1950-2015, Boletin Medico del Hospital Infantil de Mexico, 2016;73(5):302-308.
5.) R.M. McAdams, E.A. Mair, M Rajnik; Neonatal suppurative submandibular sialadenitis: Case report and literature review. Int. J. Ped. Otorhinolaringol. 69 (2005) 993- 997.
6.) C. Klem, E.A. Mair, Four-duct ligation: a simple and effective treatment for chronic aspiration from sialorrhoea. Arch. Tool. Head Neck Surg. 125 (1999)
7.) M. Pathak, L. Yadav, L.K. Bansal; Suppurative submandibular sialadenitis in a term neonate: Is there an alternative to incision and drainage? Int. J. Ped. Otorhinolaryngol Extra 8 (2013) 69- 70
8.) Ryan RF, Padmakumar B. Neonatal suppurative sialadenitis: an important clinical diagnosis. BMJ Case Rep. 2015 May 22;2015[i][ii]
Issue: Ir Med J; Vol 112; No. 6; P955
