Doctor-Patient Communication in an Outpatient Setting
K. Mulligan1, S. Egan2, D. Brennan1, Irish Society of Gynaecological oncology Public and patient involvement group members4, Y. O’Meara5*, S. O’Toole5* (*Joint senior authors)
1. Catherine McCauley education and research institute, Eccles Street, Dublin 1
2. UCD School of medicine, Belfield, Dublin 4
3. Irish Society of Gynaecological oncology
4. Our Lady’s hospice and care services, Harold’s Cross
5. Departments of Obstetrics and Gynaecology/Histopathology, School of medicine, Trinity College Dublin, Dublin 2
Abstract
Aim
To evaluate doctor patient communication within gynaecological oncology services in Ireland.
Methods
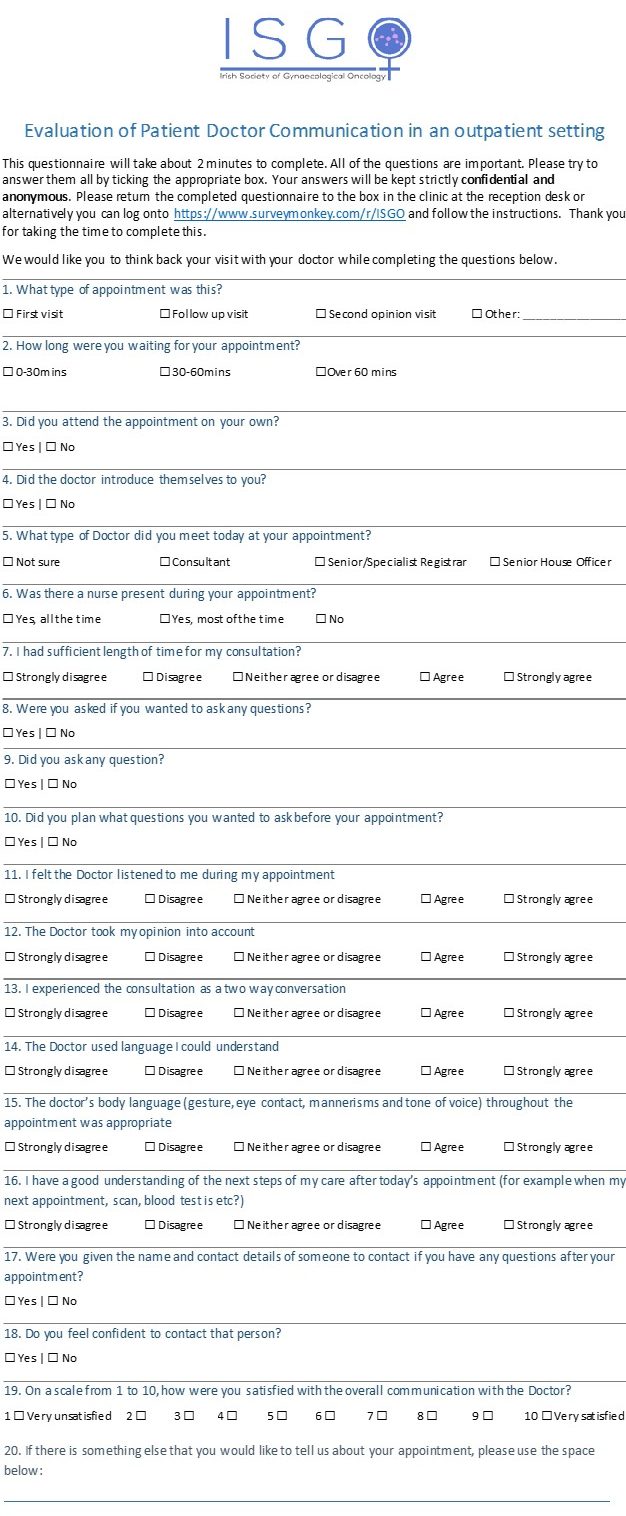
An anonymous and confidential 20 question survey was designed by the patient advocacy group ISGOPPI and distributed in three gynaecological oncology outpatient clinics in tertiary referral centres.
Results
A total of 84 patients completed the survey in the 3 Dublin hospitals. Doctors surveyed ranged from senior house officer to consultant level. Overall women were very satisfied with the communication they had received from their doctor. 85% felt that they the doctor listened to them and took their opinion into account. 84% of patients felt that the doctor’s body language was appropriate throughout the consultation. One of the main issues for women surveyed was waiting times. 33% of women waited over an hour to see their doctor and over 30% of women did not receive contact details of the clinical nurse specialist.
Conclusion
Overall our study shows that patients in gynae-oncology clinics are satisfied with the communication from their doctors. The main issues for patients were waiting times and contact details for follow up questions.
Introduction
It is widely recognised that effective doctor-patient communication plays a vital role in patient care. Doctors must aim to develop rapport and build a trusting relationship with the patient. With a focus on explanation and patient-inclusive planning as per the Calgary Cambridge Guide to the Medical Interview, doctors can ensure optimal communication with their patients.1 Effective communication leads to greater adherence with treatment, greater satisfaction with care and it has also been shown to improve health outcomes.2 We can see this reflected in gynaecological malignancy where effective physician communication skills have been shown to result in improved patient outcomes following a diagnosis.3
The Irish Society of Gynaecological Oncology is a multidisciplinary all-Ireland society focused on improving outcomes for women with gynaecological cancer which was re-established in 2016. In parallel, the Irish Society of Gynaecologic Oncology Public and Patient Involvement Group (ISGOPPI) was established “to achieve a true partnership between public/patients and the society which will promote the quantity and quality of health research and ultimately improve health services and outcomes.” The group is open to women who have or had a gynaecological cancer, significant others, professionals working within the area, members of special interest groups and the general public. The society recognises the importance of the patients’ lived experience. Women with gynaecological cancers share a wealth of knowledge and experience which can positively influence research and clinical practice.4 The implementation of patient and public involvement in research allows clinicians to improve their understanding of women’s experience and develop targeted solutions to issues that may arise throughout a patient’s journey. A growing body of evidence suggests that active patient involvement in their healthcare experience leads to better outcomes and improved cost effectiveness.5
In December 2016, the inaugural ISGOPPI workshop was held. One of the themes explored was participants views on what a true research partnership looked like within a medical setting. Patients and non-patients were divided into separate groups, deliberately to establish an undiluted patient voice. Each group provided very different interpretations of the question. The dominant theme that emerged from the patient group centred around doctor-patient communication, in particular the doctor’s body language. The findings were delivered to the PPI group, it was decided to explore this further through a national doctor patient survey.
Communication and counselling skills are widely accepted as important factors in the overall holistic management of cancer.6 Opportunities to ask questions and perceived empathy are shown to improve the patient experience so a strong emphasis should be placed on these in the consultation.7 The aim of this study was to evaluate patient doctor communication in an outpatient setting in order to understand the communication issues highlighted by the ISGOPPI and to highlight areas for improvement.
Methods
The ISGO PPI Group identified doctor-patient communication as an area that needed major improvement at their inaugural meeting in December 2016. The twenty-item questionnaire was developed in line with social constructionism theory which is based on the notion that meanings are established in coordination with others rather than separately and that individuals make sense of their world though the interactions with others.8 The theme and language of each of the twenty questions used was co-constructed with the PPI though group discussion in subsequent meetings. The survey was distributed in gynaecological oncology outpatient clinics in three tertiary referral hospitals from January-August 2018. Patients who wished to participate in the survey were informed of the survey either by a research assistant or the clinical nurse specialist and completed the survey after their consultation. Analysis of anonymised data was performed in Microsoft Excel. Ethics approval was received from all hospitals involved.
Results
Eighty-four patients completed the survey in 3 centres between January 1st and August 1st 2018. Twenty one percent of women attended for their first visit, 79% for a follow-up visit, 91% attended on their own. Thirty five percent of patients were seen by the consultant, 47% by the specialist registrar and 18% by the senior house officer.
Overall, women were very satisfied with the communication they had received from their doctor; 78% of the women surveyed felt that they had enough time for their consultation and 85% felt that the doctor listened to them and took their opinion into account. Seventy six percent of women experienced the consultation as a two-way conversation with 94% receiving an introduction from the doctor. Eighty percent of the women were given the opportunity to ask questions; 81% asked questions and 65% of these women had pre-planned the questions they wished to ask. Seventy percent of women ranked their satisfaction with the overall communication with the doctor at 10/10.
“I really appreciate being given plenty of time to talk about scans and treatment, sometimes needing to go back over things. Both professionals who talked to me today made very helpful observations and made the experience so positive.”
...
Eighty four percent of patients felt that the doctor’s body language was appropriate throughout the consultation and that the doctor used appropriate language they could understand. Eighty two percent of women felt they had a good understanding of the next steps in their care.
“Very friendly and informative. Couldn't be better.”
...
Conversely, 22% of women felt they did not have enough time in their consultation and 24% felt that the consultation wasn’t a two-way conversation.
“I feel the patient is forgotten. We are important, we live with the disease.”
...
Having a nurse present for the consultation, or even having knowledge that a gynae-cancer nurse specialist was available was an issue; 39% had a nurse present for the entire consultation, 27% had a nurse present for some of the time and 34% did not meet a specialist nurse.
“I was never introduced or given any details or even made aware of the specialised gynaecology oncology nurse. Only after my last appointment with a new consultant did I meet the nurse. It was a revelation. I only wish I had met her 3 years ago. All along I felt isolated and made to feel no one could be bothered.”
...
Seventy percent of women were given the name and contact details of someone to contact if they had any questions after their appointment and 69% felt confident enough to contact that person.
“Have never felt so looked after and cared about the entire way through my treatment.”
...
However, 30% of patients were not given the name and contact deals of someone to contact with any further questions they might have after their appointment which was a point of frustration.
“…very frustrating having to chase information yourself.”
...
One of the main issues for women surveyed included long waiting times in clinics with 55% of women waiting over 30 minutes and 33% of women waited over an hour to see a doctor.
“…why don't they give patient exact appointment times instead of giving everyone a general time and making them wait. It takes half a day to attend clinic…”
...
Discussion
Communication is of paramount importance for women undergoing treatment for gynaecological malignancies and this study highlights the importance of allowing women to play a role in shaping services for future patients. Overall the results from the survey showed 70% of the women were very satisfied (“10/10”). This was quite a high standard in comparison to the European Network of Gynaecological Cancer Advocacy Group (ENGAGe) patient survey conducted in 2017 which had only 44.7% of women describing their consultation as “very good and clear”.9 This survey, titled “What patients want to tell their doctors” was carried out in 10 European countries (Czech Republic, Denmark, Germany, Great Britain, Greece, Hungary, Poland, Serbia, Spain and Turkey) and surveyed 1436 patients.
Body language was identified by the ISGOPPI as an important factor in communication. This study showed an 84% satisfaction rate in doctor’s body language. The National Patient Experience Survey conducted by the Health Information and Quality Authority (HIQA) in Ireland and published in 2017 did not address body language as an element of patient satisfaction.10 Body language comprises over 50% of the communication a patient receives from their physician and so we would recommend this be assessed in larger Irish patient cohorts in future projects.1
There were, however, some pitfalls identified. Fifty five percent of women were left waiting over 30 minutes to see a doctor and 33% of women waited over an hour. This is something that could be improved by the allocation of specific appointment times for women. The burden of treatment time should not be overlooked as long waiting times are negatively correlated with patient satisfaction.11 Therefore reducing waiting times would reduce patient frustration and improve satisfaction levels following a consultation.
Twenty two percent of women felt they did not have enough time within their consultation. Whether this can be attributed to a lack of resources or to a lack of efforts of further communication is difficult to clarify. Comparably this is better than the national average as the National Patient Experience Survey 2017 carried out in Ireland found that 40% of people said they did not always have enough time to discuss their care and treatment with a doctor.10 The “Every Woman Study” (World Ovarian Cancer Coalition) found that over 50% of women they surveyed reported spending less than 15 minutes with the doctor when they were receiving their life-altering diagnosis of ovarian cancer.12 Whilst our study was not surveying the consultation at the time of diagnosis it is hard to contemplate delivering this information in an empathetic and sympathetic manner in 15 minutes. This data highlights the need to re-examine how doctors deliver important information in a patient centred manner.
One fifth of the women interviewed in our study were not offered the opportunity to ask questions and interestingly 35% of women did not plan questions before their consultation. This is an area that may require additional patient and public education as it would help women gain more from their consultation and give them greater ownership of their care. Hospitals should consider informing patients to keep a note of any questions that might arise as part of any appointment letter and should consider a public information campaign in the area.
Before the conclusion of the appointment the doctor should clarify that the patient understands what has been discussed and confirm a plan for future care. Almost one fifth of the women in our survey did not understand the next steps in their care. Provision of materials and educational information leaving an appointment would help women understand the burden of their illness and the next steps in their care. The ENGAGe study found that 68.9% received printed educational materials from their healthcare provider, however, the National Patient Survey 2017 in Ireland found that 46% of patients did not receive written information after leaving the hospital after a significant stay.9,10 In the “Every Woman Study”, they found that 37.3% of women were given written information, but only around 10% received information about living with ovarian cancer and sources of support.12
Thirty percent of women were not given a name and contact details of a health care professional they could communicate with if they had any questions after their appointment and 18% of women felt they did not understand the next steps in their care. It is critical that women in this situation are able to contact their team via a gynaecological oncology nurse specialist. It is also important to involve the patient in decision making in order to ensure they understand the next steps in their care. The National Patient Survey 2017 found that 36% of people were not involved enough in the decisions about their care and treatment compared to 18% in our study.10
Limitations to this study include the number of centres and the number of doctors assessed. Therefore, we would like to extend this study into other centres around Ireland and repeat the survey with an increased number of participants.
Patient and public involvement in research is imperative as those who have lived experience of a disease treatment pathway have a unique and invaluable perspective in recommending improvements to a service.13 This was an important inaugural piece of research for the ISGOPPI, empowering the patient group and allowing them to survey the communication issues that were important in their care. The results of this study have been relayed to the ISGO in order to improve current services.
Conflicts of Interest Statement
The authors have no conflicts of interest to declare.
Corresponding Author
Dr. Karen Mulligan
Catherine McCauley education and research institute,
Eccles Street,
Dublin 1
Email: [email protected]
References
1. Kurtz SM, Silverman JD, Benson J and Draper J. Marrying Content and Process in Clinical Method Teaching: Enhancing the Calgary-Cambridge Guides. Academic Medicine. 2003; 78(8):802-809
2. Back AL, Arnold RM, Tulsky JA, Baile WF, Fryer-Edwards KA. Teaching communication skills to medical oncology fellows. JCO. 2003;21(12):2433-2436.
3. Kuroki LM, Zhao Q, Jeffe DB, et al. Disclosing a Diagnosis of Cancer: Considerations Specific to Gynaecologic Oncology Patients. Obstetrics and gynaecology. 2013;122(5):10
4. Duffett L. Patient engagement: What partnering with patient in research is all about. Thrombosis Research. ELSEVIER. 2017;150: 113-120.
5. Noble S. Patient engagement in research: Are we really worse than orthopaedics? Thrombosis Research. ELSEVIER. 2017;150: 113-120.
6. Paraskevaidis E, Kitchener HC, Walker LG. Doctor-Patient Communication and Subsequent Mental Health in Women with Gynaecological Cancer. Psycho-Oncology. 1993;2(3):195-200*
7. Lisa M. Walton, Jeanne Reeve, Paul M. Brown and Cynthia M. Farquhar, Gynaecologic cancer patients' needs and experiences of supportive health services in New Zealand, Psycho-Oncology. 2009.19, 2, (201-208),
8. Leeds-Hurwitz, W. . Social construction of reality. In S. Littlejohn, & K. Foss (Eds.), Encyclopedia of communication theory. 2009. (pp. 891).
9. ENGAGe. Patient Survey 2017 in Europe – What patients want to tell their doctors? European Society of Gynaecological Oncology. 2017.
10. National Patient Experience Survey Program. The National Patient Experience Survey. Health Information and Quality Authority, Health Service Executive, An Roinn Sláinte. 2017.
11. Bleustein C1, Rothschild DB, Valen A, Valatis E, Schweitzer L, Jones R.Wait times, patient satisfaction scores, and the perception of care. Am J Manag Care. 2014 May;20(5):393-400.
12. World Ovarian Cancer Coalition. The Every Woman Study. World Ovarian Cancer Coalition. 2018.
13. Rose D. Patient and public involvement in health research: Ethical imperative and/or radical challenge? Journal of Health Psychology. 2013.19 (1): 149-158.
P934
