Drain Usage in Head and Neck Surgery: A National Survey of Thirty-five Surgeons across Ten Units
E Keane1, CW Fitzgerald1, DA Smyth1, MB Nataraj1, E Lang1, LJ Skinner1, MJ Donnelly1
1.University Hospital Waterford, Dunmore Road, Co. Waterford
Abstract
Introduction
Drain usage is commonplace in head and neck surgery. There is an increasing body of literature disputing their routine placement in certain procedures. The aim of this study is to explore modern-day practice in terms of drain usage and the use of haemostatic agents.
Methods
A simple questionnaire was devised and sent to 35 ENT Surgeons across 10 units nationally.
Results
There was an overall response rate of 77.1% (n=27). There was considerable heterogeneity amongst surgeons in terms of indication for insertion, how the decision is made to remove the drain and if any alternative/adjunctive haemostatic agents are being used.
Discussion
The management of drains is poorly defined and guidelines are lacking. With increased pressure on resources, the risk of infection and discomfort to the patient, further reflection is required to evaluate if careful patient selection rather than habitual drain insertion in every case is more appropriate.
Introduction
Drain usage is still commonplace in head and neck surgery, however there is an increasing body of evidence disputing their use in particular cases 1. Whilst drains are used in surgery in general to prevent such complications as haematoma, seroma, wound infection and skin flap issues, there are some disadvantages. They can be a source of discomfort for the patient and require a high level of maintenance on the ward. When left in situ for prolonged periods of time, they can provide a potential route for infection 2. Additionally, although they provide an idea of wound output there can be large discrepancies in the measurement of this amongst healthcare professionals, possibly leading them to left in for longer than necessary 3. In the ever increasing pressure on hospital resources and surgical inpatient beds, day case surgery has been growing in popularity. A haemostatic agent may be used in place of a drain in some scenarios but robust evidence for their efficacy and economic value are still lacking. The aim of our study was to assess modern practice amongst ENT surgeons in Ireland with regards usage of drains, how the decision to remove the drain was made and if any alternative agents were being used routinely.
Methods
A questionnaire was devised encompassing 9 procedures total. These were subsequently divided into various groups. Thyroid procedures (n=3) were 1) Total thyroidectomy, 2) Hemithyroidectomy and 3) Thyroglossal duct cyst excision/Sistrunks procedure. Salivary gland procedures (n=2) were simply 1) Parotidectomy and 2) Submandibular gland excision. Other procedures (n=4) captured 1) Parathyroidectomy, 2) Branchial cleft cyst excision 3) Neck Dissection and 4) Deep cervical lymph node biopsy. For each procedure we asked if drains were being used routinely, and if so, what type of drain (suction vs free drainage) We then asked when is the drain removed (Volume vs Time) and the acceptable volume/time frame for removing the drain. The final part of the questionnaire was to list any adjunctive/alternative haemostatic agents. The full questionnaire is available on request.
Results
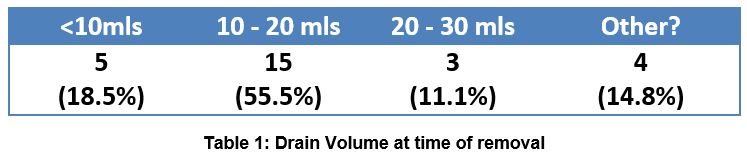
35 surgeons in 10 different centres were surveyed with a good response rate. 23 questionnaires were sent via post and this had a 69.6% response rate (16/23), while 12 were hand delivered and collected. The response rate was 91.7% (11/12). 27 surgeons were therefore included giving an overall response rate of 77.1%. The results varied considerably and by procedure type. Not all procedures were undertaken by the surgeon being asked. 12/27 of the surgeons in our survey were routinely performing total and hemithyroidectomy, and 24/27 were doing thyroglossal duct cyst excision. The results are summarised below (Fig 1)
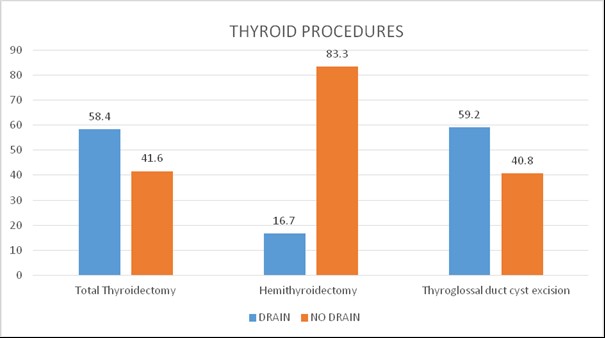
Fig 1: Graph depicting drain use in thyroid procedures (%).
Total thyroidectomy n=12/27, hemithyroidectomy n=12/27, hypoglossal duct cyst excision n=24/27
Salivary gland procedures were more universally undertaken, and drains were more frequently used. The results are summarised below:
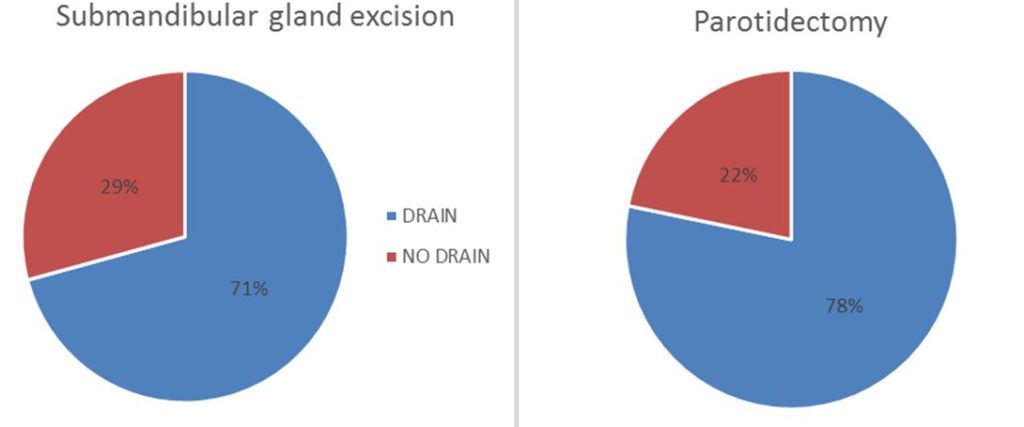
Fig 2: Pie charts depicting drain use in salivary gland surgery (%).
Submandibular gland excision n=24/27, parotidectomy n=23/27
In the miscellaneous procedure category, drain use varied by procedure type, with none of our surgeons using drains for parathyroidectomy procedures but for more extensive surgeries such as neck dissection, drains were much more frequently used. The results are summarised below:
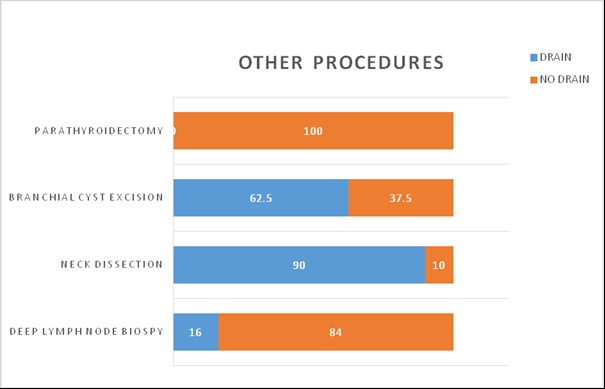
Fig 3: Graph depicting drain use in ‘other’ procedures (%). Parathyroidectomy n=9/27,
Branchial cyst excision n=24/27, neck dissection n=20/27, deep lymph node biopsy n=25/27
In all but 2 cases suction drains were preferred, with only 2 surgeons using free drainage; 1 for deep lymph node biopsy and 1 for thyroglossal duct cyst excision.
23 out of 27 surgeons decide to remove the drain depending on its volume.
2 answered not applicable, and 2 did not specify further as it was felt the variation between procedure types was too great. The preferred volumes are summarised below:
A further 12 surgeons also specified a time they deemed suitable for drain removal – 7/12 (58.3%) chose 24 hours and 5/12 chose 48 hours. Artiss was routinely used by 4 surgeons making it the most commonly used haemostatic agent. Surgicel is an agent which 2 surgeons stated they used as an adjunct to drain insertion. No other haemostatic agents were mentioned.
Discussion
Our study, the first of its kind in Europe, prompted a literature review regarding drain use in contemporary surgical practice. A shift towards shorter hospitalisations and day case procedures has become the norm in many centres globally4. There are a number of factors influencing the patient’s length of stay in all surgical disciplines, and in certain cases the use of drains has been shown to be significant 5, 6, 7, 8. The placement of drains in head and neck surgery is still commonplace in our country, and this is comparable to other surveys conducted in other countries previously 9, however, there is an increasing body of evidence disputing their use in certain procedures. Their routine use in thyroid procedures in particular has been questioned and the evidence suggests that this practice may not always be necessary. Two systematic reviews of randomized controlled trials in total thyroidectomy have been conducted, the most recent published in 2014 10. No significant difference was found between the two groups (drain vs no drain) in terms of the re-operation rate for neck haematoma (RR 1.90, 95% CI 0.87 to 4.14), transient voice change (RR 2.33 CI 0.9 to 5.96) and persistent recurrent laryngeal nerve palsy (RR 1.67 CI 0.22 to 12.51). Length of stay was significantly greater in the drain group, (Mean Difference 1.25 (0.83 to 1.68) days) as were wound infection rates and pain score. The evidence is still lacking when taking patients with coagulopathy, retrosternal goitre and other co-morbidities into consideration. Patients with independent risk factors for post-thyroidectomy bleeding such as male sex, older age, tumour size >3cm, hypertension (Systolic >150mmHg), lymph node dissection and Graves disease may require drain insertion and this can be decided on a case by case basis 11.
With advancing diagnostic practices, attempting to accurately predict histology in parotid surgery may facilitate postoperative planning and help predict the duration of drainage. This has been shown to be significantly greater in parotid malignancies when compared to benign lesions, despite undergoing the same extent of resection (p = 0.011) 12. Therefore, those patients amenable to day case surgery without the use of a drain may be identified pre-operatively.
The management of drains is ill-defined. Volume criteria was the basis for drain removal in the vast majority of the surgeons we surveyed, and this is similar to those in other specialities such as Plastic surgery 13 and Cardiothoracics 14 . If drain insertion is deemed necessary, monitoring drain outputs every 8 hours as opposed to every 24 hours has been shown to facilitate up to an additional 65% 15,16 of patients on the day after surgery without neck dissection using an acceptable drain output of less than or equal to 1ml/h. This has a beneficial effect for staff and patient alike and results in cost savings. Although it is not commonplace to discharge patients with drains in situ in the head and neck region, in some centres patients who have undergone breast surgery are discharged with their drain still in place and this has been regarded as safe and gives a high level of satisfaction 17, 18 Despite the need for increased outpatient specialist care has been deemed to be feasible with considerable resource savings 19. There are no equivalent studies regarding head and neck surgery and we have identified this as a possible area of interest for future research.
Our study demonstrates the heterogeneity of drain use in head and neck surgery in our country and this may be due in part to the advent of new haemostatic agents, obviating their use in certain cases. The safety and efficacy of these is still not supported by a large evidence base 20 and their associated complications can be severe. For example; Surgicel is an absorbable haemostat consisting of oxidized cellulose polymer may be removed or left in situ depending on the clinical need. If left in situ degradation is expected to commence within 24–48; complete degradation will usually occur between 4 and 8 weeks. 21 It can be used in the region of the recurrent laryngeal nerve during thyroid surgery for both haemostasis and as a land mark should another procedure be required 22. Surgicel has been reported to cause cell mediated type 4 hypersensitivity reactions and histiocytic reactions, and these can mimic cancer recurrence 23; abscess formation 24 and granuloma 25. However, these complications are exceedingly rare and in a case report looking back on 748 thyroidectomy patients, only 1 adverse event was documented 22. This took the form of a severe inflammatory soft tissue reaction of the skin and resolved within 3 days of removing the material. Most authors advise using it sparingly, as many cases have been attributed to use in excess 23. It costs approximately €451.95 for box of 12 (5.1cm x 7.5cm). Artiss was also mentioned by our cohort as an adjunct to drain insertion It comes frozen in 2 parts: the first being fibrinogen and the second thrombin. It mimics the final 2 stages of the coagulation cascade and the clot will continue to strengthen over 2 hours. It has been shown to significantly reduce the drain volume (to 2mls total volume) length of stay (to an average of 1 day) and hospital cost 24 When used in parotid surgery for nonmalignant disease, these tissue sealants may facilitate day case procedures without the use of drain, with savings of up to $1775 per case and a low complication rate 25.
This study also highlights the lack of specific guidelines concerning drain placement and their subsequent ward management and this will generally be left to the discretion of the operating surgeon. This may also be dependent on the level of experience of the surgeon. Following on from our study, we would encourage reflection upon current clinical practice and correlation with the evidence base accordingly. This has been illustrated particularly well in total thyroidectomy surgery where the level 1 evidence shows routine placement of drains has been shown to provide a route for wound infection and increase the patient’s length of stay without conferring any additional benefit to the patient. On review of the literature, we found that the frequency of drain output measurement may be increased in order to facilitate earlier discharge. In summary, although drains still play an important role in head and neck surgery, judicious patient selection may be more beneficial rather than habitual drain insertion in all patients.
Acknowledgements
The authors would like to thank the respondents for their time taken to fill out this questionnaire.
Conflicts of Interest
The authors hereby declare there is no conflict of interest.
Corresponding Author
Emma Keane,
University Hospital Waterford,
Dunmore Road,
Co. Waterford.
Email: [email protected]
References
1. Nimet S, Selahattin V, Mustafa Oncel, Burak D, Cem Gezen F, Baris T,Turgay E, Gülay D. Is the Insertion of Drains After Uncomplicated Thyroid Surgery Always Necessary? Surgery Today, March 2006, Volume 36, Issue 3, pp215 - 218
2. Byers RM, Ballantyne AJ, Goepfert H, Guillamondegui OM, Larson DL, Medina J. Clinical Effects of Closed Suction Drainage on Wound Healing in Patients with Head and Neck Cancer. Arch Otolaryngol. 1982;108:723-6
3. Shankla S, Bigg TC, Cox HJ, King EV. Accuracy of Drain Readings by Surgical Healthcare Professionals. Clinical Otolaryngology. Feb 2016
4. Fabricant PD, Seeley MA, Rozell JC, Fieldston E, Flynn JM, Wells LM, Ganley TJ.Cost Savings From Utilization of an Ambulatory Surgery Center for Orthopaedic Day Surgery. J Am Acad Orthop Surg. 2016 Dec;24(12):865-871
5. Li J, Li HB, Zhai XC, Qin-Lei, Jiang XQ, Zhang ZH. Topical use of topical fibrin sealant can reduce the need for transfusion, total blood loss and volume of drainage in total knee and hip arthroplasty: A systematic review and meta-analysis of 1489 patients. Int J Surg 2016 Oct; 36: 127 - 137
6. Yong L, Guang B. Abdominal drainage versus no abdominal drainage for laparoscopic cholecystectomy: A systematic review with meta-analysis and trial sequential analysis Int J Surg 2016 Nov 15;36: 358 – 368
7. Khan SM, Smeulders MJ, Van Der Horst CM. Wound drainage after plastic and reconstructive surgery of the breast. Cochrane Database Systematic Rev 2015 Oct 21;(10): CD007258
8. Kerimoglu OS, Yimaz SA, Pekin A, Icesu F, Dogan NU, Lihn TT, Celik C. Effect of Drainage on Postoperative Pain after laparoscopic ovarian cystectomy. J Obstet Gynaecol 2015 Apr;35(3):287-9
9. Williams J, Toews D, Prince M. Survey of the use of suction drains in head and neck surgery and analysis of their biomechanical properties J Otolaryngol. 2003 Feb;32(1):16-22.
10. Woods RSR, Woods JFC, Duignan ES, Timon CV. Systematic Review and Meta-Analysis of Wound Drains After Thyroid Surgery. British Journal Of Surgery 2014 DOI: 10.1002/bjs.9448
11. Chen E, Cai Y, Li Q, Chenng P, Ni C, Ji Q, Zhang X, Jin C. Risk Factors Target in Patients with Post-thyroidectomy Bleeding. Int J Clin Exp Med 2014 Jul 15;7 (7): 1837 – 44. eCollection 2014
12. Mofle PJ, Urquhart AC. Superficial Parotidectomy and Post-Operative Drainage. Clinical Medicine And Research. Volume 6. Number 2:68-71
13. Chim JH, Borsting A, Thaller S. Urban Myths in Plastic Surgery: Postoperative Management of Surgical Drains. Wounds 2016 Feb;28(2): 35-9
14. Xie HY, Xu K, Tang JX, Bian W, Ma HT, Zhao J, Ni B. A Prospective Randomized, Controlled Trial Deems A Drainage of 300ml/day Safe for Removal of The Last Chest Drain After Video-Assisted Thorascopic Surgery Lobectomy. Interact Cardiovasc Thorac Surg 2015 Aug;21(2): 200-5
15. Amir I, Morar P, Belloso A. Postoperative Drainage in Head and Neck Surgery. Annals Of The Royal College of Surgeons England, 2010. Nov;92(8): 651 – 4 DOI:10. 1308/003588410X12699662904754. Epub 2010 July 7
16. Chapman D, Purusthoman AD. Acceptability of early discharge with drain in situ after breast surgery. B J Nurs 2001 Dec 13-2002 Jan 9;10(22):1447-50
17. Holcombe C, West N, Mansel RE, Horgan K. The Satisfaction and savings of early discharge with drain in situ following axillary lymphadenectomy in the treatment of breast cancer. Eur J Surg Oncol 1995 Dec;21(6):604-6
18. Amit M, Binenbaum Y, Cohen JT, Gil Z. Effectiveness of an oxidized cellulose patch hemostatic agent in thyroid surgery: a prospective, randomized, controlled study. J Am Coll Surg. 2013 Aug;217(2):221-5. doi: 10.1016/j.jamcollsurg.2013.03.022.
19. Azmy AF. Oxidized Cellulose Haemostat Mimicking a Possible Recurrence Of Neuroblastoma. BJU International. 2001;88:295-296
20. Oxidized Cellulose (Surgicel) Mimics and Abscess After Laparoscopic Partial Nephrectomy. Actas Urol Esp. 2004. Jan;28(1):54-6
21. Cormio L, Cormio G, Di FIno G, Scavone C, Sanguedolce F, Loizzi V, Carrieri G. Oncol Lett. 2016 Aug; 12(2):1083-1084. Epub 2016 Jun 8
22. Royds J, Keiran S, Timon C. Oxidized Cellulose (Surgicel) Based Reaction Post Thyroidectomy Mimicking an Abscess: A Case Report. Int J Surg Case Rep. 2012;3(7):338-9 doi 10.1016/j.ijscr.2012.03.034
23. Ibrahim MF, Aps C, Young CP. A Foreign Body Reaction to Surgicel Mimicking an Abscess Following Cardiac Surgery. European Journal Cardio-Thoracic Surgery. 2002;22:485 -494
24. C Heffernan, K Majeed, K Davies, O Young, J Lang. Artiss in Parotid Surgery: Are Suction Drains Still Required? Report on The 55th Annual Meeting of the Irish Otolaryngology Head and Neck Society Conference 2014
25. Conroy P. Brown DH. Used of Tissue Sealant for Day Surgery Parotidectomy. J Otolaryngol Head Neck 2008 Apr;37(2):208-11
P839