Food Allergy Emergencies in Children – To what extent are Early Years Services Prepared? A cross-sectional survey
S MacGiobuin, V Stitt, D Philbin, B Higgins, G McGuire, A Marie O’Regan, M Kelly
Western Training Programme in General Practice, The Nurses Home, University College Hospital, Galway.
Abstract
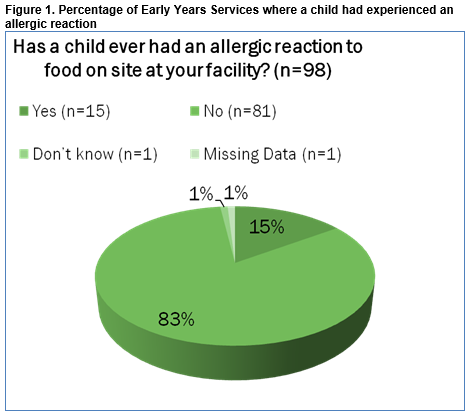
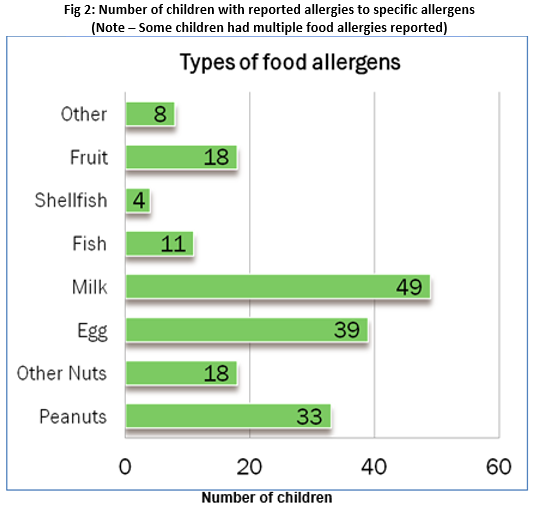
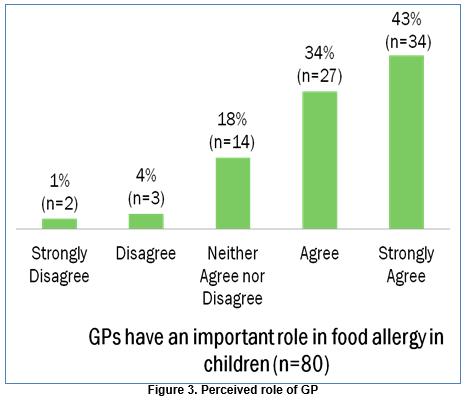
Food allergies are common in preschool children. This study’s aims are to establish prevalence, to clarify management practices, levels of preparedness and the perceived role of General Practitioners amongst Early Years Services providers. This study is an anonymous, quantitative, cross sectional study. An online questionnaire was distributed to 282 Early Years Service providers. Data were analysed using SPSS. Response rate was 35% (n=98). Prevalence of food allergy was 3% (n=119). Allergic reactions to food had occurred on site in 16% (n=15). Written emergency action plans were available in 47% of facilities (n=46). Medications were not kept on site in 63% (n=62) of facilities. General practitioners were felt to have an important role in the management of food allergies by 76% of respondents (n=61). This study identifies significant areas for improvement in the management of food allergic child in Early Years Services.
Introduction
Anaphylaxis is a serious allergic or hypersensitivity reaction that is rapid in onset and may cause death1. Anaphylaxis is under-recognised and under treated2; it can have a vague presentation and obvious skin manifestations may not be present. The goal of therapy is early recognition and treatment with adrenaline to prevent progression to life-threatening cardiorespiratory involvement. Many children with food allergies and their guardians are unsure when to use their adrenaline auto-injectors, contributing to a low quality of life and worse outcomes in the setting of an acute allergic reaction3. The estimated lifetime prevalence of anaphylaxis is 0.5-2% but recent studies confirm that the incidence of anaphylaxis, particularly food-induced anaphylaxis, is increasing worldwide4. Although any substance has the potential to cause anaphylaxis, the commonest causes of IgE-mediated anaphylaxis are: foods (particularly, peanuts, tree nuts, shellfish and fish, cow’s milk, eggs and wheat), medications (most commonly penicillin), and latex. In a series of 164 fatalities due to anaphylaxis, the median time between onset of symptoms and respiratory or cardiac arrest was 5 minutes in iatrogenic anaphylaxis, 15 minutes in stinging insect venom-induced anaphylaxis, and 30 minutes in food-induced anaphylaxis5. In case series of fatalities from food allergies among pre-school and school aged children in the United States, 9 of 32 fatalities occurred in school and were associated primarily with significant delays in administering adrenaline6. It is vital that all caregivers, including teachers, are aware of the diagnosis of anaphylaxis, recognise symptoms and are confident administering intramuscular adrenaline. School awareness of food allergy is diverse. A Turkish study showed that only 6% of the teachers reported a management plan for anaphylaxis in their schools7. A study of primary school preparedness to respond to food allergy (FA) in the West of Ireland found that 75% (24/32) of schools had at least 1 pupil attending with food allergy giving an estimated prevalence of food allergy of 1.16%8.
In Ireland, a resource pack was made available to all school facilities in 20119. There is however, no specific guidance for Irish Early Years’ Services (EYS) - an umbrella term encompassing preschool, Montessori and child-care facilities. The objectives of this study therefore were to determine the prevalence of food allergy amongst children attending EYS. Additionally, it aimed to determine current practices to manage food allergy emergencies; self-reported preparedness, knowledge and training of service providers and the perceived role of the General Practitioner (GP) in the management of food allergy emergencies.
Methods
A 32-question online survey was developed by modifying an existing questionnaire, having obtained the consent of the authors8. The questionnaire used dichotomous and free text questions along with 5-point Likert scales. The survey was piloted in two Early Years Service providers in different geographical areas prior to dissemination. The online survey tool ‘Survey Monkey’ was utilized to disseminate the survey. The study cohort was based in Galway City and County. The Child and Family Agency (TUSLA) disseminated this study to 282 Early Years Services following permission from the Data Protection Commissioner. The participants self-recruited and had two weeks to respond. Ethical approval was granted by the Irish College of General Practitioners Research and Ethics Committee. Quantitative data analysis was performed using the statistical package SPSS. Free text comments were simply reported.
Results
Demographics
The response rate was 35% (n=98). The total number of children attending these services was 3,203. Median number of children per facility was 22.5, range 2-128. The median distance from hospital was 20km (range 4-100km). 67% (n=66) reported themselves as rural. FA children had attended 74% (n=72) of services in the past. Children with FA currently attended 44% (n=43) of services. There was an average of three FA children per service (SD 2.51). Nearly 16% of EYS reported allergic reactions to food onsite – 9 of these services reporting 2 or more reactions in the past 5 years. The commonest food allergens reported in this sample were milk, egg, and peanuts. The estimated prevalence of food allergy amongst children in EYS in County Galway was 3%.
Current Management
Regarding medications, 32% of facilities stored medication for the treatment of FA on site (n=31). Of those facilities, 74% had injectable adrenaline pens (n=24), 42% had salbutamol inhalers (n=13) and 48% had antihistamines (n=15). Expiry dates on adrenaline auto injectors (AAI) were checked by staff in 70% (n=16), and by parents in 30% (n=7) of cases. In facilities that stored AAI, 83% (n=19) kept one and 13% kept two onsite (n=3). Free text comments highlighted staff reservations regarding medications: “ issues around legality of administering this medication”, “would prefer more detailed training for all staff”. Restrictions on what foods that children could bring to the facility were enforced by 66% (n=65) of EYS. Written food allergy emergency plans were in place in 47% of facilities (n=46). Of those, 55% had a plan for each individual child with food allergy (n=24). These were felt to be easy or very easy to interpret in 70% of cases (n =32). The plans were reported to have been composed by facility staff (n=26) or parents (n=9) in the majority of cases. No service reported that the plan was composed by the GP or the hospital consultant. Services who have had a child attend with FA in the past or currently are more likely to have a written food allergy emergency plan (Chi Square, p= 0.018 and 0.006 respectively).
Knowledge and Training
Training on FA or anaphylaxis was reported to have been received by 19% of facilities and an equal number, 19%, reported having no training; 3% (n=3) did not know, missing data 58% (n=57). This training was provided in 60% of cases by a healthcare professional and in some instances this was provided by TUSLA. Other training was delivered in an informal session with parents and via information leaflets and reading material. Free text comments included: “not enough talks or training given on the subject”, “Food allergy information needs to be more readily rolled out and not just sought when a child with a known allergy attends”. Using Likert Scales to assess the service providers’ perceived knowledge in relation to food allergy management, 78% agreed that staff members, in general, are aware of the symptoms of an allergic reaction. 48% agreed that staff members, in general, would know when to use an adrenaline pen. Forty-one percentagreed that staff members, in general, would know how to use an adrenaline pen. When asked would they like to receive more information on anaphylaxis management, 98% agreed, and 100% agreed that they would like more training on the subject.
The General Practitioner’s Role
Most service providers agree that “GPs have an important role in food allergy in children”, with 34% (n=27) agreeing and 43% (n=34) strongly agreeing with the statement. Eighteen percent (n=14) neither agreed nor disagreed with this statement.
Discussion
The epidemiological findings of this study were similar to those described in previous research. The prevalence of FA in children was 3%, usual quoted range 1-8%10. A study of school children in Galway showed a prevalence of just over 1%8. This difference may be explained by the fact that FA may resolve by the time children reach school age. 15% of EYS experienced a food allergic reaction on site. 20% of facilities with a FA child had experienced a reaction. These rates are similar to those described in the U.S.11. The commonest allergens identified in our study (nuts, milk and egg) were in keeping with existing data12. Areas for improvement in current management were identified. Many facilities did not store appropriate medications for FA children. For instance, only approximately half of facilities stored antihistamines. Irish Food Allergy Network (IFAN) guidelines advocate that all such children should have these medications available13. A minority of facilities stored AAI. Amongst those that did, only 13% stored two AAI. It is recommended that two AAI always be available if deemed to be indicated in case difficulty administering the first dose. The majority of services imposed food restrictions as part of the management of food allergy. The advantages and disadvantages of this approach have been described in the literature14. Although it is generally utilized and considered prudent, the findings of this study demonstrate that the practice is not universal, highlighting the need for a more uniform approach to FA in Irish Early Years Services.
Emergency plans are not universally in place for the management of FA children. Approximately half of facilities had such plans. This is a similar finding to previous studies15. With the exception of two free text comments, there was no reported input from general practitioners in the Emergency Plans. This is in keeping with the IFAN and European guidelines in this area which suggest that the majority of food allergy management is secondary care led12,16. Yet EYS providers felt that GPs have an important role in food allergy management and greater input from GPs was considered desirable. It was beyond the scope of this study to explore why service providers considered the GP so central - it may be that the local GP is the healthcare professional that they would be relying on in an emergency situation. This is worthy of further research. Yet EYS providers felt that GPs have an important role in food allergy management and greater input from GPs was considered desirable. Previous studies have showed a large variation in the levels of knowledge of staff in educational facilities regarding FA, from poor to excellent7. The findings of this study suggest service providers are confident regarding the recognition of food allergy but less confident regarding the management of reactions. There was a universal desire for further training on the subject of food allergy management which suggests that this would be an extremely receptive audience for educational material.
Regarding the strengths of this study, it highlights an important area, with no previous study of food allergy in EYS in Ireland. The stated objectives were achieved. A pilot was conducted to improve survey usability. The study built on the previous work undertaken in Primary Schools in the region, collaborating with the original researchers. Certain limitations must be acknowledged. The study focused on a limited geographical area. However, the service providers were spread over mixed urban and rural settings and varied in size. These features, along with the concordance of our epidemiological findings with the existing literature, support the generalizability of our findings. As a retrospective survey, recall bias may have influenced replies. Selection bias may have led to those with a greater interest in the area of food allergy responding to the survey. Given the limited knowledge of some providers, FA may be under recognized which may lead to an underestimation of the prevalence. The key recommendation from this study is the need for guidelines to be developed regarding the management of food allergy in EYS in Ireland. This would support early year service providers in the management of food allergies in preschool children.
Acknowlegments:
The authors wish to thank the Programme Directors and GP Trainers on the Western GP Training Programme, Galway; Dr. Edina Moylett, NUI Galway; Tusla, The Child and Family Agency and the study participants for their roles in facilitating the study.
Declaration of Conflict of Interest:
The authors report no conflict of interest.
References
1. Sampson HA, Muñoz-Furlong A, Campbell RL,Adkinson NF, Allan Bock S, Branum A, Brown SGA, Camargo CA, Cydulka R, Galli SJ, Gidudu J, Gruchalla RS, Harlor AD, Hepner DL, Lewis LM, Lieberman PL, Metcalfe DD, O'Connor R, Muraro A, Rudman A, Schmitt C, Scherrer D, Simons FE, Thomas S, Wood JP, Decker WW. Second symposium on the definition and management of anaphylaxis: Summary report - Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network Symposium. In: Annals of Emergency Medicine. 2006. p. 373–80.
2. Lieberman P, Camargo CA, Bohlke K, Jick H, Miller RL, Sheikh A, Simons FER.
Epidemiology of anaphylaxis: findings of the American College of Allergy, Asthma and Immunology Epidemiology of Anaphylaxis Working Group. Ann Allergy Asthma Immunol. 2006;97(5):596–602.
3. Kelleher MM, Dunn Galvin A, Sheikh A, Cullinane C, Fitzsimons J, Hourihane JO. Twenty four-hour helpline access to expert management advice for food-allergy-triggered anaphylaxis in infants, children and young people: a pragmatic, randomized controlled trial. Allergy. 2013;68(12):1598–604.
4. Koplin JJ, Martin PE, Allen KJ. An update on epidemiology of anaphylaxis in children and adults. Curr Opin Allergy Clin Immunol. 2011;11(5):492–6.
5. Pumphrey RS. Lessons for management of anaphylaxis from a study of fatal reactions. Clin Exp Allergy. 2000;30(8):1144–50.
6. Sampson H. Fatal and near-fatal anaphylactic reactions to food in children and adolescents. New Engl Journal of Medicine. 1992;327(6):380–4.
7. Ercan H, Ozen A, Karatepe H, Berber M, Cengizlier R. Primary school teachers ’ knowledge about and attitudes toward anaphylaxis. Pediatr Allergy Immunol. 2012;23(5):428–32.
8. Mahabir S, Gaffney C, Costello M, Villeneuve J, Moylett E. Are primary schools in the west of ireland prepared to respond to food allergy emergencies among children aged 5 to 12 years? British Society for Allergy and Clinical Immunology Abstracts of the 2013 Annual Meeting. Clinical & Experimental Allergy, 43, 1428–1472
9. Asthma Society of Ireland, Diabetes Federation of Ireland, Brainwave – the Irish Epilepsy Association and Anaphylaxis Ireland. Managing Chronic Health Conditions at School. Downloaded from http://www.anaphylaxisireland.ie/wp-content/uploads/2013/01/MCC-broc_web_revDec12-3.pdf on 17/4/16.
10. Fleischer DM, Perry TT, Atkins D, Wood RA, Burks AW, Jones SM, Henning AK, Stablein D, Sampson HA, Sicherer SH.
Allergic reactions to foods in preschool-aged children in a prospective observational food allergy study. Pediatrics. 2012;130(1):e25–32.
11. Centers for Disease Control and Prevention (CDC). "Voluntary guidelines for managing food allergies in schools and early care and education programs."Retrieved online October 5 (2013): 2014.
12. Muraro A, Agache I, Clark A, Sheikh A, Roberts G, Akdis CA, Borrego LM, Higgs J, Hourihane JO, Jorgensen P, Mazon A, Parmigiani D, Said M, Schnadt S, Van Os-Medendorp H, Vlieg-Boerstra BJ, Wickman M.
"EAACI Food Allergy and Anaphylaxis Guidelines: managing patients with food allergy in the community." Allergy. 2014;69(8):1046–57.
13. Irish Food Allergy Network. Online publication. Accessed from http://ifan.ie/medication-for-food-allergy/; Dec 10 2014
14. Young MC, Muñoz-Furlong A, Sicherer SH. Management of food allergies in schools: A perspective for allergists. J Allergy Clin Immunol. 2009;124(2):175–82.
15. Pouessel, G., A. Deschildre, C. Castelain, A. Sardet, S. Sagot‐Bevenot, De Sauve‐Boeuf, C. Thumerelle, and C. Santos. Parental knowledge and use of epinephrine auto-injector for children with food allergy. Pediatr Allergy Immunol. 2006;17(3):221–6.
16. Irish Food Allergy Network. Online publication. Accessed from http://ifan.ie/diagnosis-and-management-in-primary-and-community-care/managing/ on Dec 10 2014
(P600)