How would Mary Poppins fare in labour? Practically perfect?
Unlikely.
1,2L Bolger, 1,3RSweeney, 4M Foley, 4R Mahony
1Royal College of Surgeons in Ireland
2St Vincent’s University Hospital
3Beaumont Hospital
4National Maternity Hospital
Abstract
Introduction
Unrealistic expectations of labour in first time mothers can present challenges to physicians and midwives. This study calculated the percentage of “practically perfect” births in nulliparous women, defined as a labour without intervention, an intact perineum and a positive neonatal outcome.
Methods:
This was a retrospective study of the nulliparous deliveries that occurred in the National Maternity Hospital over two years (2014/2015). To extract the perfect births, we excluded deliveries <37 weeks, induction/pre labour Caesarean Section (CS), Artificial Rupture of Membranes (ARM), oxytocin, fetal blood sample, emergency CS/instrumental deliveries, perineal damage and suboptimal Apgar scores.
Results:
0.8% of nulliparous mothers had a practically perfect birth.
Discussion
Our results provide a useful statistic for clinicians and nulliparous mothers, which could be further validated by similar studies in similar units. The study had a large cohort which objectively quantified perfect births. Research on the subjective perception of perfect births could add value to these findings.
Introduction
Managing women’s expectations of labour and delivery can be an area of challenge for physicians and midwives. Furthermore, having expectations and outcomes equate, has been shown to be a significant predictor of maternal childbirth satisfaction1. With increasing influence of social media, there is the potential for women to feel pressure to have the “perfect” birth. This research provides useful statistics for providing realistic expectations for first time mothers.
Methods
This was a retrospective study of data collected at the time of birth from all the deliveries that occurred in the National Maternity Hospital Dublin over a two-year period, from the 1st of January 2014 to the 31st of December 2015 (n=18692). Our focus was on the 8292 nulliparous labours. The data was combined on an excel spreadsheet and the following exclusion criteria were applied in the following order:
1. Delivery <37 weeks
2. Induced/Pre labour Caesarean section
3. Artificial rupture of Membranes
4. Oxytocin
5. Fetal Blood Sample
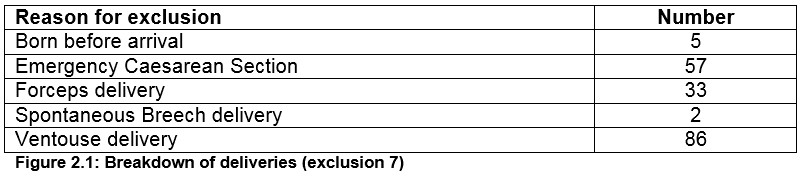
6. Emergency Caesarean section/Forceps Delivery/Ventouse Delivery
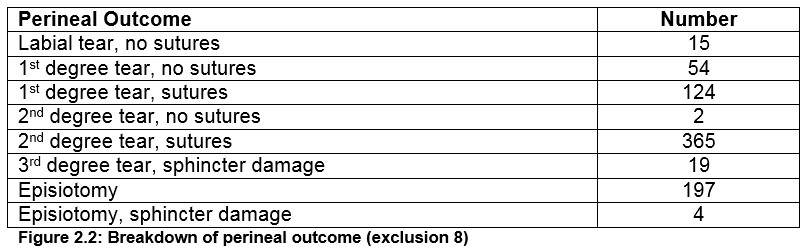
7. Perineal Outcome: first degree tear +/- sutures, Second degree tear +/- sutures, 3rd degree tear, episitomy +/- sphincter damage, labial tears
8. Neonatal Outcome: Apgars of <9 at 1 or 5 minutes
Data on the labours who opted for midwifery led care (n=482) was also analysed and the same exclusion criteria applied to this cohort. A total of n=54 deliveries were recorded as home deliveries. No ethical approval was needed as this data is published in the National Maternity Hospital’s annual report.
Results
Among 18,698 there were 8,292 nulliparous women of whom 7,616 delivered after 37 weeks. Of these, 4,171 went into spontaneous labour, while 2,753 were induced. 692 had a caesarean section as a primary procedure. Two thousand, one hundred and eleven women were noted to have an artificial rupture of membranes in labour and 857 received oxytocin. After excluding these, there were 1203 remaining. One hundred and seventy-two women had a fetal blood sample taken, leaving 1,031.
Of the 1,031 women who had a spontaneous labour without any of the interventions mentioned above, 57 had an emergency caesarean section, 86 had a ventouse delivery, 33 had a forceps delivery, two were spontaneous breech deliveries and 5 were born before arrival to hospital. That excluded a total of 183 leaving 848 practically perfect births. We then looked at the perineal outcome and exluded all tears and episiotomies leaving 68 with an intact perineum. Out of these 68, we extracted two based on suboptimal Apgar scores.
This left 66 “perfect” deliveries or 0.8% of all nulliparous mothers who had a practically perfect birth. Out of the 66 “perfect” deliveries 15 were noted to have opted for community midwife care. A total of n=482 women availed of community midwife care in 2014 and 2015. When we separated those who went with community midwife care and the standard obstetric care group, the rate of “practically perfect” births was 3% in the midwife group compared to 0.7% in the obstetric group.
Fig 1: step by step exclusion criteria 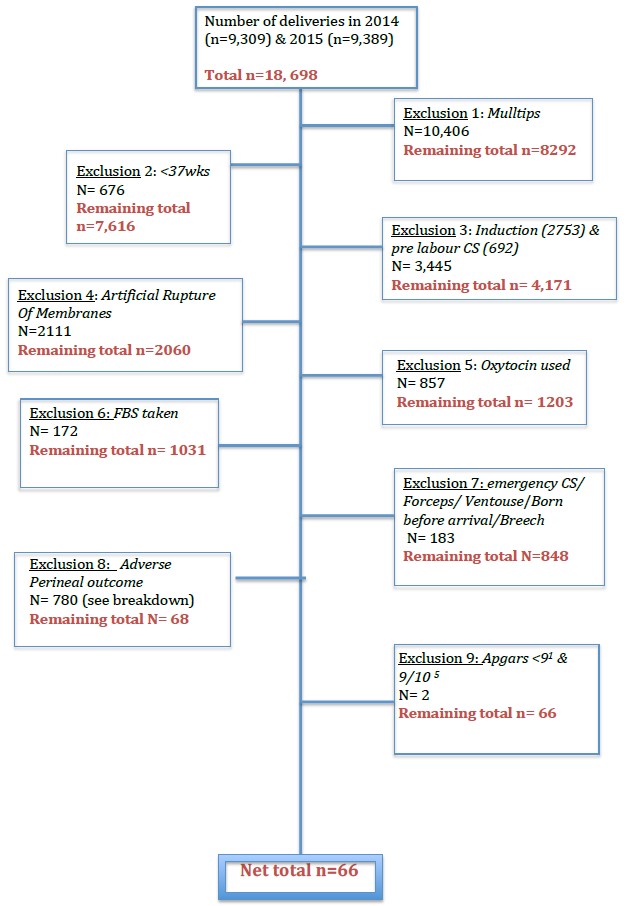
Discussion
These statistics can be useful for both clinicians and first time mothers, and could be further validated by similar studies in other maternity hospitals. This study was carried out in a maternity unit that practises active management of labour, which utilizes early amniotomy and oxytocin and has been proven to reduce the duration of labour along with the rate of caesarean section without affecting womens satisfaction with their labour and delivery2,3. In this paper we demonstrated that while there is a poor chance of a “practically perfect birth”, neonatal outcomes remain positive: with only two excluded based on Apgar scores. Of note, these Apgar scores were 8 at one minute & 9 at 5 minutes. With such a low result it is important to examine the areas of the exclusion criteria that had the greatest effect. Two of the most significant exclusion criteria were Artificial Rupture of Membranes (ARM) and perineal outcome.
If we include the 51% of the cohort that had an ARM in spontaneous labour, the proportion of practically perfect births increases to 1.4%. It can also be said that only accepting intact perineums into our practically perfect group was too stringent. When we took the objective measure of whether mothers required sutures or not and included labial tears, first degree tears without sutures and second degree tears without sutures, the number of practically perfect births doubles (1.6%). Interestingly if the same applications are made to the midwifery led cohort, the percentage rises from 3% to 6%. This is potentially an area for future research. However, it is important to note that midwifery-led services are reserved for the lowest risk mothers. While there was a significant difference between the rate of practically perfect births in the midwifery led cohort compared to the obstetric cohort, statistical comparison would not be practical due to the small number in the midwifery group (n=482).
The study included those who received epidurals during their labour (n=19/66 practically perfect births). Neither antenatal nor postnatal complications were included. This is a potential limitation to the study. In this study, we objectively defined a practically perfect birth resulting in a stringent exclusion criteria. We received no input from the mothers themselves which is both a limitation and an area for future research. Studies into the maternal perception of a perfect birth could add value to this research. This is an astonishing result which would be interesting to see compared to other maternity hospitals and midwifery led units throughout the country and internationally.
Importantly, the question following this research must be asked; would imparting this information to first time mothers evoke fear of labour or provide realistic expectations?
Conflict of Interest
There is no conflict of interest to declare in this study
Corresponding Author’s Details
Dr Lucy Bolger, Royal College of Surgeons in Ireland
Email: [email protected]
References
1. Goodman P, Mackey MC, Tavakoli AS. Factors related to childbirth satisfaction. Journal of Advanced Nursing 2004; 46(2) http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2648.2003.02981.x/abstract (accessed 18 October 2016)
2. Lawrence Impy, Peter Boylan. Active Management of Labour revisited. BJOG: An International Journal of Obstetrics and Gynaecology 1999; 106(3)
3. Sadler LC, Davison T, McCowan LM. Maternal satisfaction with active management of labour: a randomized control trial. Birth; Issues in Perinatal Care 2001;28(4) http://onlinelibrary.wiley.com/doi/10.1046/j.1523-536X.2001.00225.x/abstract (accessed 18 October 2016)
(P756)
