Investigating the Barriers to the Uptake of Diabetic RetinaScreen
GH Bennett1, A Tuthill2
1 School of Medicine, University College Cork
2 Department of Endocrinology, Cork University Hospital
Abstract
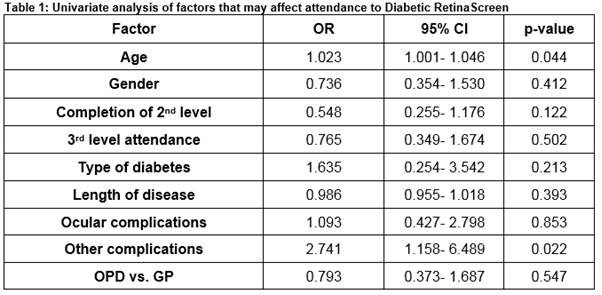
Diabetic retinopathy is a significant complication of diabetes, and the most common cause of blindness in people under the age of 65. The National Diabetic Retinal Screening Programme (Diabetic RetinaScreen) was established to detect sight threatening retinopathies. The purpose of this cross-sectional study is to determine the barriers to the uptake of Diabetic RetinaScreen, to investigate discrepancies in attendance, if any, between patients whose diabetes care is delivered in a large tertiary referral hospital out-patient setting or in general practice, and to evaluate general practitioner’s satisfaction with the service. Older age (OR 1.023, 95% CI 1.001 to 1.046) and complications of diabetes, excluding ocular complications, (OR 2.741, 95% CI 1.158 to 6.489) were associated with increased attendance at Diabetic RetinaScreen. Online referral is now available and the preferred method of referral. Efforts to encourage younger patients who do not yet have complications of diabetes may be beneficial.
Introduction
Diabetes is a condition characterised by chronic hyperglycaemia. This hyperglycaemia is caused by insulin deficiency, an element of insulin resistance, or a combination of both. The two main types of diabetes are Type 1 and Type 2 diabetes mellitus. Type 1 is less common and generally presents in childhood, the pathogenesis involves destruction of β-cells (the insulin secreting cells of the pancreas), therefore leading to an absolute insulin deficiency. Type 2 usually presents in the older population with an element of insulin resistance as well as a relative insulin deficiency. In Ireland and worldwide, type 2 diabetes is increasing in prevalence due to our aging population as well as our rising rates of obesity1. This increase in diabetes within the population has significant ramifications with regards morbidity and mortality. Diabetes can cause a host of macrovascular and microvascular diseases including diabetic retinopathy, diabetic nephropathy, diabetic neuropathy and accelerated coronary artery disease. Diabetic retinopathy and maculopathy are two serious microvascular complications of diabetes resulting from poor glycaemic control. Diabetic retinopathy is a disease process which progressively damages the retina, the part of the eye that is sensitive to light, leading to a characteristic visual field defect known as a scotoma, and eventually blindness. Studies have shown that diabetic retinopathy is the leading cause of blindness globally. One third of patients with diabetes have signs of diabetic retinopathy. This was approximately 126.6 million people with diabetic retinopathy in 2010, a figure which is growing each year6. In the initial stages diabetic retinopathy is asymptomatic but can be detected by carrying out a retinal exam2. Furthermore, approximately one third of all cases of diabetic retinopathy are sight threatening. Therefore, screening for retinopathy is imperative in all patients with diabetes to prevent vision loss.
Methods
Ethical approval was sought and granted by the Clinical Ethics Committee of the Cork Teaching Hospitals (CREC) to perform this quantitative cross-sectional study. It included three populations: a random sample of general practitioners in Cork, and patients with diabetes who either attended Cork University Hospital (CUH) diabetes outpatients, or general practice. Two questionnaires were developed for this study, one for general practitioners and the second for patients. Questionnaires were mailed to 100 randomly selected general practitioners with stamped return envelopes. Patient questionnaires along with a consent form were distributed and collected in diabetes outpatients in CUH and in three general practices. The patients included in this study were all over the age of 16, had diabetes, and gave informed consent. The study was conducted between June 2015 and October 2015.
Results
In total 147 patients (102 from Out Patients Department (OPD) and 45 from general practice) and 72 practitioners responded and were included in this study.
General Practitioner Survey
There was a 76.6% (72/94) response rate from general practitioners. Only 55.6% (40/72) were happy to refer their patients to Diabetic RetinaScreen, this was mainly due to the time required to call the service. The most popular referral method was online registration (53%, 38/72), followed by a phone call (18%, 13/72), e-mail (17%, 12/72), and a letter (14%, 10/72). Although not included in this questionnaire, 11% (8/72) of general practitioners proposed that patients refer themselves to the service. Sixty-eight out of 72 (94.4%) GPs were satisfied with the outcome of the service. As of April 2015 an online referral system is available for patients, however it does require the GP to submit a registration form in conjunction with the online application.
Patient Survey
Ninety-three out of 147 (63.3%) patients surveyed had already attended a screening appointment while 91.2% (134/147) were aware of Diabetic RetinaScreen. Eighty-five out of 147 (57.8%) patients surveyed preferred the current location of screening i.e. community, rather than hospital appointments. There was no statistically significant difference found between the patients attending CUH diabetes outpatient clinics (n=102) and patients attending their general practitioners (n=45) regarding attendance at the screening programme (OR 0.793, 95% CI 0.373 to 1.687). Only two factors were identified as having an impact on attendance; older age (OR 1.023, 95% CI 1.001 to 1.046) and non-ocular complications of diabetes (OR 2.741, 95% CI 1.158 to 6.489), were associated with increased attendance rates. Other areas examined that did not impact on attendance were: gender, completion of second-level education, third-level attendance, type of diabetes, length of disease, and ocular complications of diabetes (Table 1).
The most significant barrier to attendance identified by patients was that they were already attending the hospital eye clinic (n=15). The other barriers reported were other (not specified), travel, time, and inconvenience.
Discussion
The majority of general practitioners were unhappy with the current referral system in place in 2015, as they considered a phone call inconvenient and time consuming, suggesting that other methods such as online registration or patient self- referral should be considered. As of April 2015 Diabetic RetinaScreen has introduced a new referral system which comprises of an online patient registration system along with a registration form completed by the patients GP. The most significant barrier to attendance at Diabetic RetinaScreen reported by patients is that they are already attending the hospital for screening appointments and did not wish to attend another appointment. Indeed, some patients may have been advised that attendance at Diabetic RetinaScreen was not required for another year as they had already been seen in the hospital eye clinic. Previous studies3,4 although carried out in different populations, have shown social deprivation to negatively impact attendance rates. This study did not examine social deprivation. However, educational level was examined. There may be a correlation between social deprivation and educational levels5 with some suggestion that lower levels of education correlated with a reduced likelihood to attend screening. Despite this, the research carried out for this project analysed education levels and determined that educational levels did not impact attendance of the studied population. Increasing age and complications of diabetes (excluding ocular complications) were associated with an increased likelihood to attend screening. Older age is also associated with increased attendance in the literature3. This could be used to reinforce the benefits of screening particularly in younger patients and those who have not yet developed complications of diabetes. Diabetes and its complications are now pandemic in this country. Measures such as Diabetic RetinaScreen are greatly needed to manage these complications. It appears to be successful thus far with the majority of patients attending their appointments. However, education relating to diabetic retinopathy screening should be targeted towards patients at risk of developing diabetic retinopathy (younger patients and those with pre-existing complications of diabetes). The new online referral system which allows patients to register themselves should also facilitate an increase in the numbers of patients referred to, and as a result, screened by Diabetic RetinaScreen.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Correspondence:
Gillian Bennett, School of Medicine, University College Cork, College Road, Cork.
E-mail: [email protected]
References
1. Velma Harkins. A Practical Guide to Type 2 Diabetes Care. HSE; 2008. https://www.hse.ie/eng/services/Publications/topics/Diabetes/A_Practical_Guide_to_Integrated_Type_II_Diabetes_Care.pdf
2. NHS. Complications of Diabetes: Screening for Retinopathy Management of Foot Ulcers. 1999 5(4): https://www.york.ac.uk/media/crd/ehc54.pdf
3. Orton E, Forbes-Haley A, Tunbridge L, Cohen S. Equity of uptake of a diabetic retinopathy screening programme in a geographically and socio-economically diverse population. Public Health. 2013; 127(9): 814-821. http://www.publichealthjrnl.com/article/S0033-3506(13)00130-3/abstract
4. Scanlon PH, Carter SC, Foy C, Husband RF, Abbas J, Bachmann MO. Diabetic retinopathy and socioeconomic deprivation in Gloucestershire. Journal of Medical Screening. 2008; 15(3): 118-121. http://journals.sagepub.com/doi/abs/10.1258/jms.2008.008013
5. van Eijk KN, Blom JW, Gussekloo J, Polak BC, Groeneveld Y. Diabetic retinopathy screening in patients with diabetes mellitus in primary care: Incentives and barriers to screening attendance. Diabetes Research and Clinical Practice. 2012; 96(1): 10-16. http://www.diabetesresearchclinicalpractice.com/article/S0168-8227(11)00626-7/abstract
6. Yingfeng Zheng,Mingguang He, Nathan Congdon. The worldwide epidemic of diabetic retinopathy. Indian J Ophthalmol. 2012 Sep-Oct; 60(5): 428–431. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3491270/
(P628)