Irish Policy-makers’ Perceptions of Barriers and Facilitators to Hand Hygiene Compliance
C. Madden1,3, S. Lydon2,3, K. Lambe1,3, P. O’Connor1,3
1. Department of General Practice, School of Medicine, National University of Ireland, Galway, Ireland
2. School of Medicine, National University of Ireland, Galway, Ireland
3. Irish Centre for Applied Patient Safety, National University of Ireland, Galway, Ireland
Abstract
Aim
To examine the barriers to, and facilitators of, hand hygiene (HH) practices as perceived by national and hospital-level HH policy-makers in Ireland; and identify the extent to which the issues identified are addressed in national HH guidelines.
Methods
Semi-structured interviews were conducted with 12 national-and hospital-level Irish HH policy-makers. Four national Irish HH policy documents were reviewed.
Results
The policy-makers identified a range of barriers and facilitators of HH compliance. These were found to fit into six themes, with a number of suggestions for how to improve HH compliance. All of the policy documents referenced the World Health Organization’s five moments, but lacked guidance on how to improve HH compliance beyond recommending audit and feedback.
Conclusion
Policy-makers identified potential areas for targeting in future interventions. The varied extent to which the issues identified in the interviews were addressed in the guidelines, policies, and standards suggest that revision of such documents is required.
Keywords: Hand hygiene; guidelines; stakeholder evaluation; patient safety.
Introduction
In Ireland, preventing Healthcare Associated Infections (HCAIs) has been identified as a system-wide priority area of the Health Services National Service Plan1. HH is considered the primary means of preventing HCAIs2-4. However, international HH compliance rates are poor, with estimations of around 40% compliance5 in hospital settings. Therefore, there is a need to understand variables that impact upon HH.
Although a number of studies have examined perceived barriers and facilitators of front line healthcare workers (HCWs) to HH compliance5-7, the opinions of HH policy-makers have not been examined to the same extent, despite being in a stronger position than front line HCWs to influence HH compliance policies8.
The purposes of this study were to: (1) examine the barriers to, and facilitators of, hand hygiene practices perceived by national and hospital-level HH key policy-makers in Ireland; and (2) identify the extent to which the issues identified in the interviews with the HH policy-makers are addressed in national Irish HH guidelines, policies and standards.
Methods
Seven interviews were conducted with national-level policy-makers (four nurses and three doctors who can influence national-level HH policies), and five with hospital-level policy-makers (two nurses and three doctors who can influence hospital, or healthcare group level HH policies). Interviews were conducted until it was judged that data saturation had been reached for each of the two groups of policy makers. Interview prompts were based upon the COM-B ('capability', 'opportunity', 'motivation'- behaviour') model of behaviour change9. Ethical approval was obtained from Galway University Hospitals Research Ethics Committee.
Interviews were carried out between July and December 2017. Participants returned their consent form via email or post. Interviews were conducted by telephone and were audio recorded and transcribed. The interview data was analysed using a deductive content analysis approach10. The COM-B model9 was used as the initial framework for coding the data. Two coders read all the interview transcripts, coded the interviews against the COM-B model, and compared their coding of the data until consistent coding was achieved. Changes to the COM-B model were made through discussion and consensus.
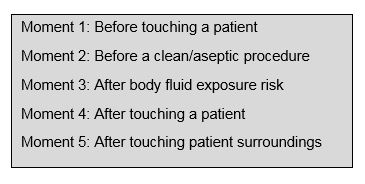
Google© was used to identify Irish health service guidelines, policies, and regulations relating to HH. Websites of relevant Irish health organisations and agencies and Irish hospital groups were also searched in order to identify additional potentially relevant material. The search was limited to documents published since 2009, the year in which the WHOs HH guidelines, including the ‘five moments for hand hygiene’ (see Figure 1) were published11. The approach to searching was based on a previously used internet based search method12. In order to be included, guidelines had to: (a) be published by government or non-governmental organisations at a national-level within Ireland; (b) describe standards or guidelines for appropriate HH practices in a healthcare setting; and (c) be the most current version of the document. A structured approach was used to extract information from the guideline documents and assess the extent to which the documents addressed the themes identified from the stakeholder interviews. Data extraction and theming was conducted by two of the authors and any disagreements were resolved through discussion until consensus was reached.
Figure 1. Five moments for hand hygiene11
Results
Interviews
The mean interview length was 19 minutes 58 seconds (SD=8 minutes 11 seconds). Examples of the themes and subthemes that emerged are presented in Figure 2, and descriptive exemplar quotes from the interviews are shown in Table 1.
Figure 2. Themes and subthemes emergent from the thematic analysis.
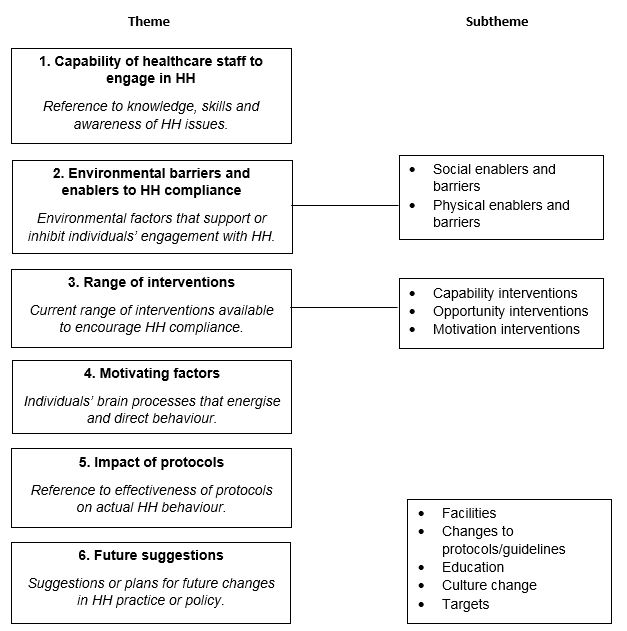
Table 1. Themes, sub-themes, and descriptive examples for interview data.
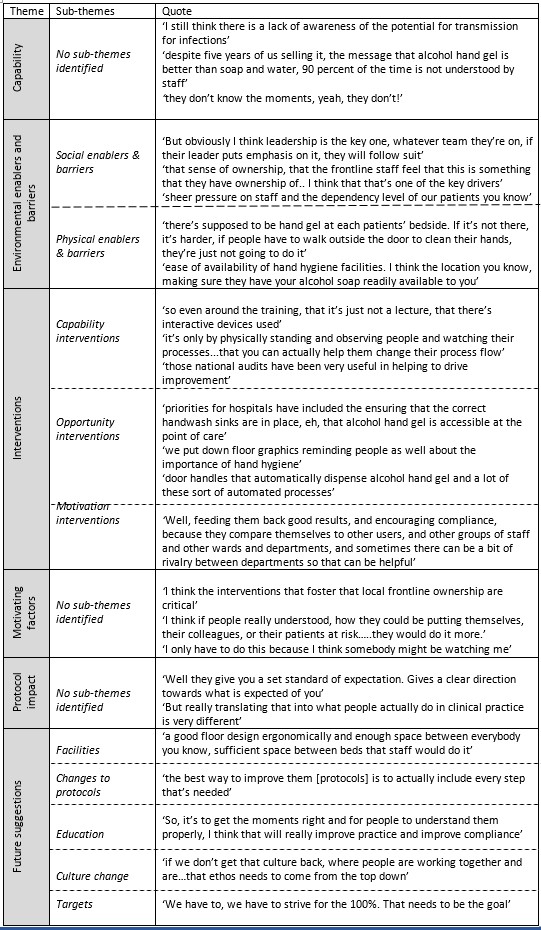
Theme 1. Capability of HCWs to engage in HH.
Capability refers to individuals’ psychological or physical ability to enact a particular behaviour9. Interviewees frequently expressed the opinion that there was a lack of knowledge, skills and awareness of HH issues amongst HCWs (see Table 1).
Theme 2. Environmental enablers and barriers to HH compliance.
This theme had two subthemes: social enablers and barriers and physical enablers and barriers (see Figure 2). Effective leadership and a sense of ownership of HH interventions amongst frontline staff was identified as a crucial social enabler of HH compliance by participants. Unfavourable working conditions characterised by understaffing, overcrowding and lack of HH facilities were identified as barriers to HH compliance.
Theme 3. Range of interventions.
This theme had three subcategories (see Figure 2). Participants described capability interventions which aimed to promote or improve knowledge, skills and awareness of HH issues (see Table 1). The most frequently mentioned such intervention was the provision of education and training to HCWs. Opportunity interventions were also identified, and constituted those that aimed to improve the social and physical environment in support of HH compliance. These mostly related to the provision and accessibility of supplies and facilities. Lastly, participants described motivation interventions, key among these being the performance of audits and feedback. Punitive approaches were considered to be effective in some cases (e.g., refusing staff their car parking passes if they had not completed HH training).
Theme 4. Motivating factors.
A range of motivating factors that prompt staff to engage in appropriate HH behaviour were identified by interviewees, including perceived importance, consequences of poor compliance, perceived surveillance, and perceived prioritisation (see Table 1).
Theme 5. Impact of protocols.
Interviewees had mixed responses regarding the impact of HH protocols on behaviour (see Table 1). Whilst some participants believed them to be useful for providing clear instruction and direction regarding expectations and regulations, others felt that there was inadequate information provided on the specific HH moments and felt they did little to actually improve HH, suggesting there exists a discrepancy between protocols and translation into clinical practice.
Theme 6. Future suggestions.
A number of suggestions to improve HH practice and policy in the future were made by the interviewees, relating to protocols, education, culture change, facilities, and targets. Table 1 provides examples of suggestions from interviewees in these areas.
Document analysis
Four documents were determined to meet the inclusion criteria (See Table 2). Documents were developed by a range of healthcare organisations including subgroups of the Royal College of Physicians Ireland group on HCAI and antimicrobial resistance (AMR)13-15, the Irish College of General Practitioners15, and the Health Information and Quality Authority (HIQA)16.
Table 2. Summary of content of included Irish hand hygiene guidance.
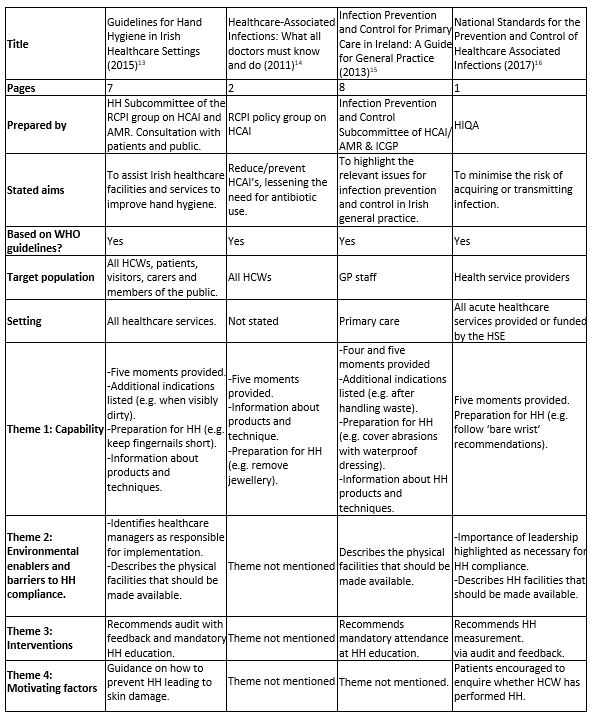
Three of the guidelines’ focus was on infection control13-15, with sections on HH embedded within. One guideline16 was centred exclusively on HH. One document was developed based on previous guidelines13, another16 was developed following a review of the literature and existing guidelines, and an extensive consultation exercise involving key stakeholders. The remaining documents14,15 did not provide any information on their development process. All of the documents made reference to the WHO’s five moments11.
Four of the six themes identified from the interviews were also present in the guideline documents. The impact of protocols and future suggestions themes were not present in the four documents reviewed. As shown in Table 2, information related to the capabilities theme was identified in all of the documents (e.g., details of the HH moments, products and techniques). Environmental enablers and barriers to HH compliance was identified in three of the documents, with two providing advice on physical enablers, and two discussing both physical and social enablers. In relation to Theme 3, two documents addressed the range of interventions by advising the use of audit and feedback and HH education, while one mentioned education only. Motivating factors was identified in two guidelines; one provided information on prevention of skin damage, and another provided advice on encouraging patient enquiry.
Discussion
HH compliance is regarded as the primary means of preventing HCAIs2-4. This study sought to explore the perceptions of national- and hospital-level policy-makers in the Irish health service relating to HH compliance, and its barriers and facilitators, and identify the extent to which the barriers and facilitators reported by these individuals are addressed in national Irish HH guidelines, policies and standards.
Ownership and leadership were the most notable enablers of HH compliance mentioned by the interviewees. There is a large body of literature to support the need for positive social influences17. The importance of social enablers was also acknowledged in one of the guidelines in the document analysis, suggesting that ‘leaders at all levels support and encourage colleagues to adhere to good hand hygiene practices by leading by good example’16. Future HH interventions could harness these factors to improve HH. Strategies that incorporate leading by example (e.g., ‘the executive walk-around’18,19) are effective strategies for engaging frontline staff8. Despite this, in a recent review of interventions to improve HH compliance20, modelling was not used in any of the included studies. Further research is required to determine the resource intensity and cost-effectiveness of such strategies in order to render them tenable as long-term solutions20.
Interviewees also frequently noted a lack of knowledge, skills and awareness of HH issues amongst Irish HCWs. In particular, they suggested that there was lack of understanding of the link between HH and infection transmission, and ‘when’ to perform HH rather than ‘how’. Recommendations for strategies on how to improve HH compliance, and related teaching, are also lacking from the HH documents reviewed- likely a result of the absence in research evidence. Systematic reviews have consistently found poor quality of research concerning which strategy, or combination of strategies, are effective in improving HH compliance20,21. Consistent with the document analysis, the main motivational intervention recommended by interviewees was the performance of audits and provision of feedback. However, it has been suggested that a refocus towards HH programmes and delivery of targeted interventions may be a more effective strategy than an ‘obsession with auditing’22. Although direct observation can assist behaviour change (e.g., improving compliance)23, addressing commonly perceived barriers to compliance, such as aforementioned ambiguity amongst HCWs, could add further value to the auditing process24.
The policy-makers recognised that procedure and protocols alone have limited utility in improving HH compliance. Suggestions for improving the use of protocols included using ‘stories’ to apply the five moments to specific situations within various HCW roles. Adapting the five moments to specific care situations has been previously identified as a useful improvement strategy8. Additional suggestions made by interviewees for improving HH compliance included the provision of adequate facilities and appropriate ergonomic space, greater education efforts surrounding HH compliance, and increasing HH targets. Changing the culture was also noted as a potential area for change, with policy-makers emphasising the importance of involving management and leaders in promoting HH practice.
This study had a number of limitations. First, this study explored policy-maker perceptions of barriers and facilitators to HH compliance; it could be argued that because policy-makers are operating at a higher level, their perceptions of the exact difficulties experienced may not be in alignment with the practice experiences of HCWs25. Nevertheless, all of the interviewees were, or had been, front line HCWs. Second, only national-level guidelines were examined, which may have resulted in the exclusion of potentially useful hospital-level guidelines. However, the difficulty in systematically accessing hospital-level guidelines precluded their inclusion. Finally, only Irish HH guidelines were reviewed. However, the scope of this study was to consolidate HH guidelines in an Irish context exclusively as there is clear value in examining these issues at a national level.
Conclusion
Policy-makers are in a strong position to influence policy and guidance on HH. Examination of their perceptions provides a valuable insight regarding the areas that could be targeted for improvement in future interventions. The varied extent to which the issues identified in the interviews by HH policy-makers were addressed in the national Irish HH guidelines, policies and standards suggest that refinement and revision of such documents is required.
Funding:
Funding for this research was obtained from the Irish Health Research Board.
Conflict of Interest:
The authors have no conflicts of interest to declare.
Corresponding Author:
Dr. Paul O’Connor
Post: Department of General Practice,
National University of Ireland,
1 Distillery Road,
Co. Galway,
Ireland.
Email: [email protected].
Telephone: + 353 91 492897
References
[1] Health Service Executive. National Service Plan 2012.
[2] Pittet D, Boyce JM. Hand hygiene and patient care: pursuing the Semmelweis legacy. The Lancet Infectious Diseases. 2001; 1:9-20.
[3] Pittet D, Allegranzi B, Sax H, Dharan S, Pessoa-Silva CL, Donaldson L, Boyce JM. Evidence-based model for hand transmission during patient care and the role of improved practices. The Lancet infectious diseases. 2006; 6(10):641-52.
[4] Kretzer EK, Larson EL. Behavioral interventions to improve infection control practices. American Journal of Infection Control. 1998; 26(3):245-53.
[5] Erasmus V, Daha TJ, Brug H, Richardus JH, Behrendt MD, Vos MC, van Beeck EF. Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infection Control & Hospital Epidemiology. 2010; 31(3):283-94.
[6] Pittet D, Simon A, Hugonnet S, Pessoa-Silva CL, Sauvan V, Perneger TV. Hand hygiene among physicians: performance, beliefs, and perceptions. Annals of internal medicine. 2004; 141(1):1-8.
[7] Sax H, Allegranzi B, Uckay I, Larson E, Boyce J, Pittet D. ‘My five moments for hand hygiene’: a user-centred design approach to understand, train, monitor and report hand hygiene. Journal of Hospital Infection. 2007; 67(1):9-21.
[8] McInnes E, Phillips R, Middleton S, Gould D. A qualitative study of senior hospital managers’ views on current and innovative strategies to improve hand hygiene. BMC infectious diseases. 2014; 14(1):611.
[9] Michie S, Van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation science. 2011; 6(1):42.
[10] Elo S, Kyngäs H. The qualitative content analysis process. Journal of advanced nursing. 2008; 62(1):107-15.
[11] Safety WP, World Health Organization. WHO guidelines on hand hygiene in health care. 2009.
[12] Godin K, Stapleton J, Kirkpatrick SI, Hanning RM, Leatherdale ST. Applying systematic review search methods to the grey literature: a case study examining guidelines for school-based breakfast programs in Canada. Systematic reviews. 2015; 4(1):138
[13] HH Subcommittee of the RCPI group on HCAI and AMR. Guidelines for hand hygiene in Irish healthcare settings. 2015.
[14] Royal College of Physicians Ireland. Healthcare-Associated Infections: What all doctors must know and do. 2011.
[15] Lemas H, McDonnell N, O’Connor N, Rochford S. Infection prevention and control for primary care in Ireland: A guide for general practice. 2013.
[16] Health Information and Quality Authority. National standards for the prevention and control of healthcare-associated infections in acute healthcare services. 2017.
[17] Dyson J, Lawton R, Jackson C, Cheater F. Development of a theory-based instrument to identify barriers and levers to best hand hygiene practice among healthcare practitioners. Implementation Science. 2013; 8(1):1.
[18] Parand A, Dopson S, Vincent C. The role of chief executive officers in a quality improvement initiative: a qualitative study. BMJ open. 2013; 3(1):e001731.
[19] Weaver SJ, Lubomksi LH, Wilson RF, Pfoh ER, Martinez KA, Dy SM. Promoting a culture of safety as a patient safety strategy: a systematic review. Annals of internal medicine. 2013;158:369-74.
[20] Lydon S, Power M, McSharry J, Byrne M, Madden C, Squires JE, O’Connor P. Interventions to improve hand hygiene compliance in the ICU: a systematic review. Critical care medicine. 2017; 45(11):e1165-72.
[21] Gould DJ, Moralejo D, Drey N, Chudleigh JH, Taljaard M. Interventions to improve hand hygiene compliance in patient care. Cochrane database of systematic reviews. 2017(9).
[22] McLaws ML, Azim S. Doctor, do you have a moment? National Hand Hygiene Initiative compliance in Australian hospitals. The Medical journal of Australia. 2014; 201(5):265.
[23] Jeanes A, Coen PG, Wilson AP, Drey NS, Gould DJ. Collecting the data but missing the point: validity of hand hygiene audit data. Journal of hospital infection. 2015;90:156-162.
[24] Jeanes A, Coen PG, Gould DJ, Drey NS. Validity of hand hygiene compliance measurement by observation: A systematic review. American journal of infection control. 2018;000:1-10.
[25] Tsui L, Chapman SA, Stewart S. A handbook on knowledge sharing: Strategies and recommendations for researchers, policy makers and service providers. Alberta: Community-University Partnership for the Study of Children, Youth, and Families; 2006.
P914
