Isolated Unilateral Pulmonary Artery Agenesis complicated by Symptomatic Aspergilloma
A Daly1, C Gunaratnam2, K C Redmond1, D Eaton1
1Professor Eoin O’Malley National Cardiothoracic & Transplant Unit, Mater Misericordiae University Hospital, Eccles Street, Dublin 7, Ireland
2Department of Respiratory Medicine, Beaumont Hospital, Beaumont, Dublin, Ireland
Abstract
Isolated unilateral pulmonary artery agenesis is a rare diagnosis. Poor blood flow to the lung parenchyma renders the tissue susceptible to opportunistic infections. We present the unusual case of isolated unilateral pulmonary artery agenesis complicated by aspergilloma. Management options and considerations are discussed.
Introduction
Isolated unilateral pulmonary artery agenesis (IUPAA) is a rare diagnosis, which renders the affected lung susceptible to opportunistic infection such as aspergillus fungal infection. Surgical resection is the only definitive treatment of aspergillomas but can prove hazardous and requires meticulous planning, especially in the setting of IUPAA1,2. With this in mind, we present the very rare, and second only reported case of isolated unilateral pulmonary artery agenesis complicated by ipsilateral aspergilloma.
Case Report
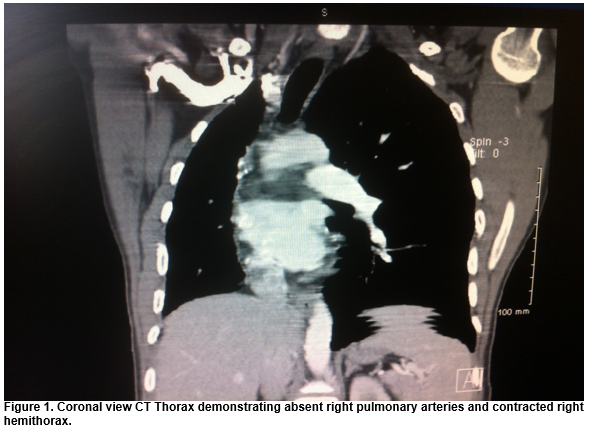
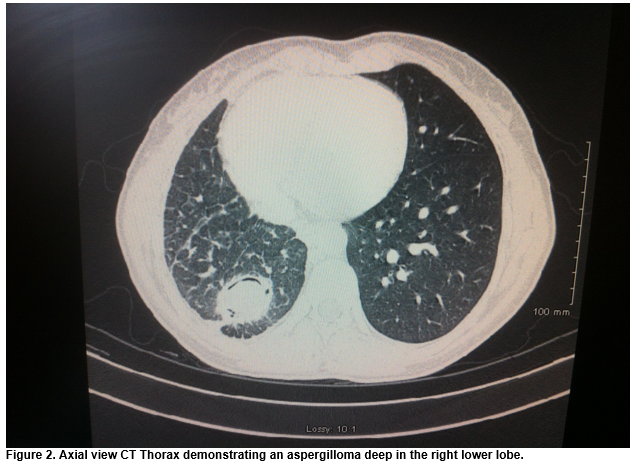
A 34-year-old female presented with recurrent lower respiratory tract infections and haemoptysis secondary to a longstanding symptomatic right lower lobe aspergilloma. CT Thorax demonstrated congenitally absent right pulmonary arteries, congenital right hypoplastic lung, a contracted right hemithorax and mycetoma located deep within the right lower lobe (figures 1-2). The inferior and superior pulmonary veins were both present and of normal architecture.
Initially, the patient was treated conservatively, however, symptoms progressed to such an extent that her quality of life was severely affected and surgical management was opted for. A right lower lobectomy was performed via thoracotomy. Adhesions between the lung and chest wall were less than anticipated. Significant ectatic bronchial arteries were noted, clipped and divided. The inferior pulmonary vein was stapled and divided using a vascular stapler. The fissure was completed and bronchus divided using staples. The phrenic nerve was injected with lidocaine to temporarily paralyse the diaghram and reduce the residual space. The patient recovered well, with no acute complications. She was discharged 11 days post surgery. She remains well with no complications or sequelae two years post operatively.
Discussion
Unilateral pulmonary artery agenesis (UPAA) is a rare congenital defect often associated with congenital cardiac defects such as patent ductus arteriousus or Tetralogy of Fallot. Less frequently, UPAA occurs in isolation. IUPAA often remains asymptomatic, presenting as an incidental finding in adulthood. Alternatively, multiple aortopulmonary collateral arteries (MAPCAs) may develop and result in haemoptysis. Pulmonary hypertension and ventilation of non-perfused lung may contribute to and result in significant V/Q mismatch. Furthermore, poor arterial blood supply in tandem with underlying conditions such as bronchiectasis, render the lung susceptible to recurrent and opportunistic infections including fungal infections such as aspergillus.
Pulmonary aspergillomas are most commonly found in patients with immunodeficiency or underlying lung pathology. Aspergilloma may present incidentally, with haemoptysis or with extrapulmonary visceral abscesses as a result of embolization. Mass diameter of more than 18mm and cavity diameter of greater than 22mm are associated with a significantly increased risk of massive haemoptysis3. Surgical resection is the only definitive treatment for mycetomas and is indicated most commonly for haemoptysis1. The use of pharmacotherapy has not demonstrated significant improvement in either morbidity or mortality2.
In this case, the patient required intervention for management of severe and potentially life-threatening haemoptysis. The aim of surgery was to remove the aspergilloma without leaving a cavity or potential residual infected space. Wedge resection was unsuitable due to location of the mycetoma. Right lower lobectomy of the lesion was considered to be the most appropriate surgery, with a salvage option of proceeding to bilobectomy if required. We wished to avoid pneumonectomy due to risks of long term space infection. Consideration was given to collateral vessels which may result in increased bronchial artery flow (up to 17% of total cardiac output) thereby significantly increasing the risk of bleeding4. Large MAPCAs can be coiled or embolized preoperatively to reduce the risk of blood loss5. In this case, preoperative contrast-enhanced CT imaging did not identify any large MAPCAs. Recurrent and chronic infection can result in extensive adhesions which can make dissection difficult and increase risk of haemorrhage. Fortunately, in this case, adhesions were less than expected. Finally, the phrenic nerve was temporarily paralysed in order to reduce the volume of the post-lobectomy space and reduce the potential risk of empyema.
This case reports the successful surgical management of IUPAA and concurrent symptomatic aspergilloma. The report serves to highlight to the audience the surgical concerns and consideration regarding this diagnosis. Meticulous planning and exploration of all surgical options is required.
Corresponding Author
Adam Daly, Mater Misericordiae University Hospital, Eccles Street, Dublin 7
Email: [email protected]
Tel: 00353 803 2000
Conflict of Interest
The authors declare no conflicts of interest
References
[1] Khan MA, Dar AM, Kawoosa NU, Ahangar AG, Lone GN, Bashir G, Bhat MA, Singh S. Clinical profile and surgical outcome for pulmonary aspergilloma: nine year retrospective observational study in a tertiary care hospital. Int J Surg [Internet]. 2011 Jan [cited 2014 Aug 11];9(3):267–71. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21252003
[2] Sagan D, Goździuk K. Surgery for pulmonary aspergilloma in immunocompetent patients: no benefit from adjuvant antifungal pharmacotherapy. Ann Thorac Surg [Internet]. 2010 May [cited 2014 Aug 7];89(5):1603–10. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20417786
[3] Lee J-K, Lee YJ, Park SS, Park JS, Cho Y-J, Park YS, Yoon HI, Lee CT, Lee JH. Clinical course and prognostic factors of pulmonary aspergilloma. Respirology [Internet]. 2014 Jul 3 [cited 2014 Aug 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/24995570
[4] Kadir IS, Thekudan J, Dheodar A, Jones MT, Carroll KB. Congenital unilateral pulmonary artery agenesis and aspergilloma. Ann Thorac Surg [Internet]. 2002 Dec [cited 2014 Aug 11];74(6):2169–71. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12643413
[5] Redmond KC, Mansfield L, Griffin N, Mullen M, Dusmet M. Coiling of major aortopulmonary collateral arteries with agenesis of the left pulmonary artery prior to pneumonectomy. Ann Thorac Surg [Internet]. 2009 Jan [cited 2014 Aug 11];87(1):312–4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19101325
(P656)