Management of Paediatric Buckle (Torus) Wrist Fractures in Irish Emergency Departments: A National Survey
A. Abdelhady, A. Ahmed, E. Umana, J. O’Donnell
Department of Emergency Medicine, University Hospital Galway, Galway
Abstract
Buckle fractures are the most common wrist fractures reported in the paediatric age group. National Institute for Clinical Excellence (NICE) recommends using a non-rigid immobilisation with no follow up for these patients and appropriate discharge advice. A telephone survey was conducted to assess the variation in practice in Irish hospitals regarding the mpediatrianagement of buckle fractures. Twenty eight centres that manage paediatric patients with trauma were contacted. This survey demonstrates that over 70% (>20) of centres in Ireland are managing buckle fractures using the traditional approach of backslab cast and follow-up in fracture clinic. Despite relevant research and NICE guideline recommendations, there is a slow adoption of current evidence among Irish hospitals which points to a need for a national consensus on management of buckle fractures.
Introduction
Wrist fractures are a frequent reason for presentation to the Emergency department (ED) in the paediatric population. Buckle fractures account for 50% of distal radius fractures and are said to be stable fractures given the intact cortex on both sides1,2. Conventional X-ray of the forearm is considered gold standard for detection and guiding management of buckle fracture, though ultrasound use is rapidly gaining popularity among ED doctors3. Management of buckle fractures, varies greatly among studies in the literature, but traditionally, it is managed with a backslab cast and fracture clinic review4. National Institute for Clinical Excellence (NICE) recommends using a splint and no follow-up required after appropriate discharge advice has been given5. The aim of this survey was to assess the variation in practice in Irish hospitals regarding the management of buckle fractures.
Methods
A telephone survey was conducted of all Irish centres receiving paediatric patients with trauma. The survey was conducted from April to June 2017, where the doctors in charge of EDs and Minor Injury units were contacted about the management of buckle fractures in their respective departments. The survey contained four domains: one Diagnostic modality (X-ray vs Ultrasound), two Current departmental guidelines on the management of buckle fractures (back slab vs wrist splint), three Follow-up of patients (Fracture Clinic vs ED Review Clinic vs General Practitioner (GP)), four Discharge advice policy (written or verbal). The survey questionnaire can be found in the supplementary material.
Results
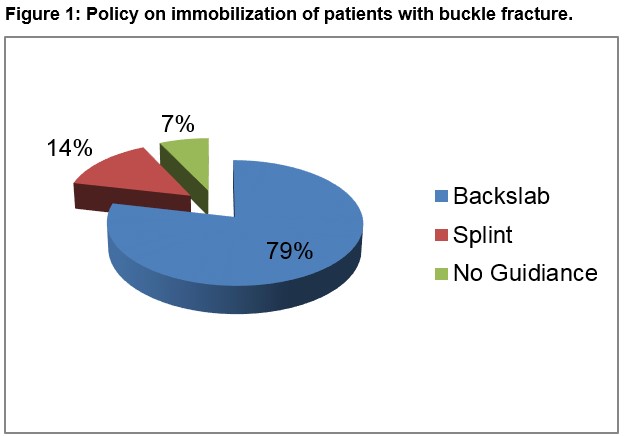
There are 44 hospitals and 11 minor injury units in Ireland, of which 28 centres manage paediatric patients with trauma. All 28 centres were contacted and responded to the survey. Ultrasound was used as diagnostic modality in four (14%) centres. In these centres ultrasound was performed by ED consultants during day time hours, otherwise the child underwent an x-ray of the forearm as part of diagnostic work up. Twenty-two (79%) centres managed buckle fractures with back slab cast, four (14%) centres with splints and two (7%) with no clear guidance (Figure 1). Follow-up was via Fracture Clinic in 21 (75%) centres with the remainder being followed-up by GP's (four (14%)) or review clinics (three (11%)). Twenty (71%) centres had written discharge advice policy, 7 (25%) centres gave verbal advice only and one centre had no clear policy.
Discussion
This survey demonstrates that over 70% of centres in Ireland are managing buckle fractures using the traditional approach of back slab cast and follow up in fracture clinic. Plint et al more than a decade ago conducted a survey of ED doctors and orthopedic surgeons working in 8 hospitals in Canada as regards the management of buckle fractures1. They demonstrated a substantial variability between hospitals and doctors when it comes to management of buckle fractures1. A recent meta-analysis found non-rigid immobilisation methods to be more advantageous than rigid cast regarding better functional recovery, lower incidence of complications or problems and lower cost4. Callender et al reported a possible estimated annual savings of €18,596.00, when soft cast immobilisation with no fracture clinic follow up and written advice given upon discharge was implemented in their institution6. Their study was carried out in an Irish hospital with annual paediatric attendance of 32,000 patients. Only four centres were using ultrasound for diagnostics purposes, which could indicate presence of ultrasound consultant leads propagating its use. With sensitivity and specificity approaching 97% and 95% respectively, ultrasound can be helpful as first line modality in diagnosis of buckle fractures under strict policies and protocols3. Current evidence along with NICE recommendations suggest that using wrist splint and no follow up after written discharge advice has economic and resource implications which are of benefit4,5. This survey highlights the slow adoption of current evidence among Irish hospitals and points to a need for a national consensus on management of buckle fractures.
Conflict of Interest
The authors declare that they have no competing interests.
Correspondence:
Dr Ahmed Abdelhady, Registrar, Department of Emergency Medicine, University Hospital Galway, Galway
Email: [email protected]
Reference
1 Plint A, Clifford T, Perry J, Bulloch B, Pusic M, Lalani A, Ali S, Nguyen BH, Joubert G, Millar K. Wrist buckle fractures: a survey of current practice patterns and attitudes toward immobilization. Cjem. 2003;5(02):95–100.
2 Randsborg P-H, Sivertsen EA. Distal radius fractures in children: substantial difference in stability between buckle and greenstick fractures. Acta Orthopaedica. 2009;80(5):585–9.
3 Hamer DD-D, Blanker MH, Edens MA, Buijteweg LN, Boomsma MF, Helden SHV, Mauritz GJ. Ultrasound for Distal Forearm Fracture: A Systematic Review and Diagnostic Meta-Analysis. Plos One. 2016;11(5).
4 Jiang N, Cao Z-H, Ma Y-F, Lin Z, Yu B. Management of Paediatric Forearm Torus Fractures. Paediatric Emergency Care. 2016;32(11):773–8.
5 Fractures (non-complex): assessment and management [Internet]. Guidance and guidelines | NICE. [cited 2017Oct29]. Available from: https://www.nice.org.uk/guidance/ng38.
6 Callender O, Koe S. Using softcast to treat torus fractures in a paediatric emergency department. Irish Medical Journal. 2015;108(4).
P793
