Knife to Skin Time in Orthopaedics- A New Sub-Speciality Selection Tool
R Stewart, K McDonald, A Adair
Orthopaedic department, Musgrave Park Hospital, Stockmans lane, Bt9 7JB
Abstract
Several selection methods have been used to aid selection into orthopaedic training programs but no process exists to aid in sub-speciality selection. A process which is continuous, unbiased and encompasses technical skill and decision making would be the gold standard. This paper analyses the use of a daily clinical task that assesses many of the desirable traits of a prospective trainee. A retrospective review of 13,474 orthopaedic procedures was under taken. The results showed a clear distinction between orthopaedic sub-specialities in time taken to perform this task. The authors suggest that this could provide a low cost insight into the appropriate subspecialty for orthopaedic trainees.
Introduction:
Multiple studies have attempted to determine which attributes are predictive of success during specialist training as well as the optimal method of selecting trainees who possess these attributes. Factors that are consistently ranked as being important in the selection of candidates into orthopaedic programs across the world include; performance during orthopaedic rotation, postgraduate exam scores, medical school class rank, interview performance, and letters of recommendation1,2,3,4,5. A variety of selection instruments have been used to admit the most promising applicants to training programs. These instruments range from cognitive selection tools such as aptitude tests or the selection instruments to non-cognitive selection tools such as regular interviews, reference letters and psychometric questionnaires. The reliability and validity of these selection instruments differs widely.
A “halo effect’ has been well documented in the literature which suggests that during a one off interview a trainee can appear more competent that may be the case6,7. These papers supported the use of continuous assessment as a scoring tool. During the final years of higher orthopaedic training trainees must decide which sub-specialty they would like to pursue. For some trainees this is straightforward though no assessment tool has been developed to help trainees identify which area they might be best suited. During the 19th century, surgical hand preparation consisted of washing the hands with antimicrobial soap and warm water. In 1939, a 7-minute handwash with soap, water, and a brush, followed by 70% ethanol for three minutes after drying the hands with a towel and finally in the second half of the 20th century, the recommended time decreased from >10 minutes to 5 minutes8.
This study aims to identify if the need to provide advice on subspecialty selection in othropaedic surgery could be satisfied by well-documented, continuous assessment tool which all trainees must before on a daily basis - hand washing.
Methods:
This retrospective study reviewed all consultant performed orthopaedic procedures that took place in one calendar year (1st January 2014- 31st December 2014) at Musgrave park hospital, a district general hospital in Northern Ireland that specialises in elective othropaedic surgery. Using the theatre management system, BOIS and a standardised template the difference between the “patient positioned and ready” and “ knife to skin” time (the time taken to wash your hands) was compared.
Data collected included; the type of procedure, the subspecialist interest of the consultant, the time the patient was draped and ready and finally the time the procedure was started. The data for each subspecialty was then correlated and an average time calculated. Inclusion criteria: all general anaesthetic procedures logged on the theatre management system on an elective orthopaedic list. Exclusion criteria: joint injections, closed procedures and all procedures performed under local anaesthetic.
Results:
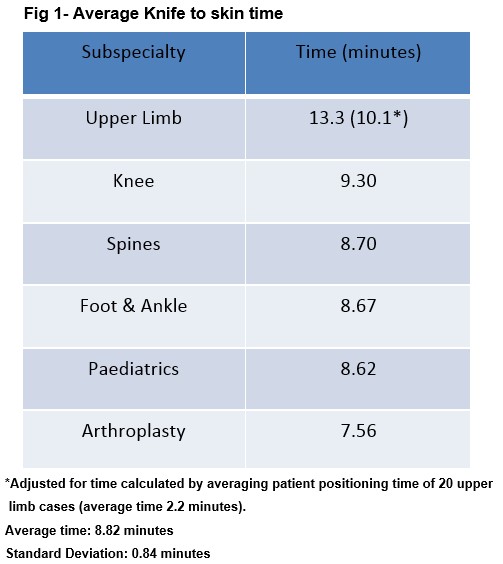
A total of 13,437 orthopaedic procedures were performed within the data collection period. With joint injections and closed procedures (1,858) subtracted the final number was 11,579 procedures. Six discrete orthopaedic subspecialties were identified; upper limb, knee, spine, foot and ankle, paediatric and arthroplasty. All specialities fell within two standard deviations of the average with the exception of upper limb surgeons, who took on average 34% (2.54 minutes) longer to wash their hands.
Discussion
To correctly wash one’s hand prior to a surgical procedure requires many of desirable attributes that training programs try to identify at interview. It requires; knowledge (of the correct aseptic liquid and technique), attention to detail (to cover the require steps), manual dexterity (to efficiently complete the steps) and professionalism (to ensure the risk of infection to your patient is minimised). A retrospective analysis allows for a form of continuous assessment (removing the ‘halo’ effect) and prevents the presence Hawthorne effect. (a type of observation bias in which a subject who knows their being observed changes their behaviour).
The authors feel that the time taken to wash surgeon’s hands is an indicator of the future orthopaedic sub-speciality of a trainee and provides a low cost analysis of the key attributes of a successful trainee. If it takes you longer than 10 minutes to wash your hands you could be destined to be an upper limb surgeon.
Contact Details:
Orthopaedic department, Musgrave Park Hospital, Stockmans lane
Email: [email protected]
Conflict of interest:
No conflicts of interest were identified. No funding was received for the publication of this paper.
References
1. Gallagher AG, Leonard G, Traynor OJ. Role and feasibility of psychomotor and dexterity testing in selection for surgical training ANZ J Surg. 2009 Mar; 79(3):108-13
2. Tansley P, Kakar S, Withey S, Butler P.Ann. Visuospatial and technical ability in the selection and assessment of higher surgical trainees in the London deanery.R Coll Surg Engl 2007; 89: 591–595
3. Egol KA, Collins J, Zuckerman JD. Success in orthopaedic training: resident selection and predictors of quality performance. J Am Acad Orthop Surg. 2011 Feb; 19(2):72-80
4. Gilbart M, Cusimano M, Regehr G. Evaluating surgical resident selection procedures. Am J Surg. 2011 Mar: 181(3);221-225
5. Raman T, Alrabaa R, Sood A, Maloof P, Benevenia J, Berberian W. Does residency slection criteria predict performance in orthopaedic surgery residency. Clin Orthop Relat Res (2016) 474;908-914
6. Stephenson-Famy A, Houmard B, Oberoi S, Manyak A, Chiang S. Use of interview in the resident candidate selection: a review of the literature. J Grad Med Educ; 2015 Dec; 7(4): 539-548
7. Brustman L, Williams F, Carroll K, Lurie H, Ganz E, Langer O. The effect of blinded versus nonblinded interviews in the resident selection process.J Grad Med Educ: 2010 Sep; 2(3): 349-353
8. Widmer AF, Manfred R, Voss Andreas.Surgical hand preparation: state of the art.J Hosp Infection (2010) 74, 112e122
(P741)
