National Survey Of The Aetiological Assessment Service Of Permanent Childhood Hearing Loss In Ireland
J. Balfe 1,4, N. Van Der Spek 2,5, D. Waldron 3,5
1. Department of Neurodisability and Developmental Paediatrics, Tallaght University Hospital
2. Department of Paediatrics, Cavan General Hospital, Co Cavan
3. Department of Paediatrics, St Luke’s General Hospital, Kilkenny.
4. Discipline of Paediatrics, Trinity College Dublin
5. Department of Paediatrics, Royal College of Surgeons in Ireland, Dublin
Abstract
Aim
The Universal Neonatal Hearing Screening Programme (UNHS) was implemented nationally in 2014. All infants identified with permanent childhood hearing loss (PCHL) should have a paediatric assessment performed. This survey aimed to assess available paediatric services and to inform service development.
Methods
All paediatricians involved in assessment of infants with PCHL were identified. A questionnaire was developed using the BAAP standards. Results were collated on excel.
Results
Thirty-three paediatricians assess children with PCHL, only 18% (6/33) had received specific training. Waiting time for assessment was beyond the recommended timeframe in the majority of cases (mean 14.4 weeks, range 2-52). Timely access to services such as MRI, genetics and ophthalmology was limited.
Conclusion
The survey highlights significant deficits in the paediatric component of the UNHS. A model of regionalisation with recommendations to improve the paediatric skill set, resources and supporting services is suggested.
Introduction
Best practice indicates that all children who are identified with permanent childhood hearing loss (PCHL) should have access to prompt paediatric assessment to determine the need for aetiological investigations[i]. Early paediatric assessment allows the identification and management of potentially treatable causes e.g. congenital CMV (cCMV) infection and provides an opportunity to prevent or reduce disability. It also allows the identification of associated co-morbidities including potentially fatal cardiac arrhythmias. The role of the paediatrician also includes liaison with agencies including tertiary specialist services, education, disability services and other community based organisations[ii] .
The Universal Neonatal Hearing Screening program (UNHS) first piloted in Cork in 2011, was implemented nationally in 2014[iii]. In 2016, 106 infants were identified with PCHL in Ireland, an incidence of 1.66 per 1,000 babies screened.[iv] In addition to the infants identified at birth with PCHL, there are an estimated equal number of older children with later diagnosis, who also require a paediatric assessment.
The roll-out of the UNHS programme did not include funding for paediatric services and no new consultant posts with a dedicated PCHL role have been developed. A 2015 external audit of the National Screening programme performed in 2 regions identified significant gaps in the provision of the paediatric component of the assessment [v]. In response to this audit a national survey of paediatricians involved in the evaluation of children with PCHL was performed to further assess services available nationally and to inform service development.
Methods
All paediatricians involved in the aetiological assessment of infants with PCHL were identified from the national audiology lead. There are no audio-vestibular physicians in Ireland and thus the survey was limited to paediatricians who in their absence are generally accepted to be the most appropriate professionals to complete the aetiological assessment2. A questionnaire (available on request) was developed using the British Association of Audiovestibular Physicians (BAAP) guidelines[i] and with reference to the gold standards audited in the 2015 external audit[ii]. The questionnaire was sent by post with a covering letter and followed up with email reminders.
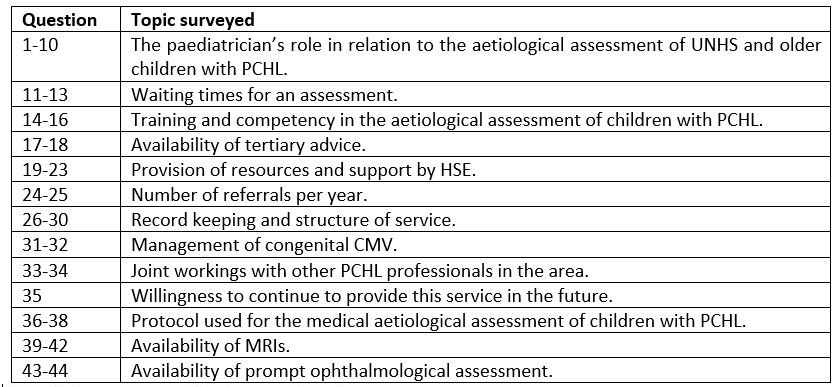
Table 1: Areas surveyed in the questionnaire
Results
Thirty-eight consultant paediatricians, working in 18 units, were identified and received a questionnaire. The response rate was 97.4%, the single non-responder had retired. 46% (17/37) of responders were general paediatricians, 46% (17/37) were general paediatricians with a special interest in community child health and there was one neonatologist, one paediatrician with a special interest in inherited metabolic disorders and one paediatric endocrinologist. A total of 33 paediatricians reported involvement in the aetiological assessments of infants identified through the UNHS, on older children referred through other pathways or both. Twenty-five (76%) paediatricians who reported assessing children with PCHL were based at a maternity unit.
The audit identified significant national variability in waiting times for paediatric assessment from 2 weeks to 52 weeks. The average waiting time to see an infant identified with hearing loss via the UNHS programme was 14.4 weeks. Considering the time required to confirm PCHL, waiting time to see a paediatrician should be few days to facilitate the diagnosis and treatment, if indicated, of otherwise asymptomatic children with cCMV and to allow performance of MRI internal auditory meatus (IAM) and brain under natural sleep, avoiding sedation or a general anaesthetic[viii]. It is recognised that it is important to identify and treat cCMV infection within 6 weeks of age[ix] but only eight paediatricians (24.2%) reported that they could do the assessment within that timeframe. Less than 28.6% reported a clear referral pathway to an infectious disease service to ensure rapid processing of cCMV cases.
Standards indicate that professionals assessing children with PCHL should be appropriately trained and competent[x] however only 18.1% (6/33) paediatricians who do the assessments report having received specific PCHL training while only 21% (7/33) of paediatricians believed that they saw sufficient throughput of infants/children with PCHL to retain clinical expertise.
Access to tertiary support and second opinions was limited, 54.5% (18/33) paediatricians reported adequate opportunity to seek advice (radiology and genetics excluded) for a complex PCHL infant/child if required, typically from local ENT or regional/tertiary ENT colleagues. Thus nearly half reported limited access to tertiary advice for complex cases. The majority (71.4%) reported concern that resource limitation could pose a serious risk if missed/delayed diagnosis.
Only 2 out of the 33 paediatrics doing the assessments hold a database of patients referred and assessed. The reported average number of infants with PCHL identified through the UNHS seen by the paediatrician for aetiological assessment per year was 7.3 infants, varying between 0 and 32 infants per year. Four paediatricians were unable to estimate the numbers seen.
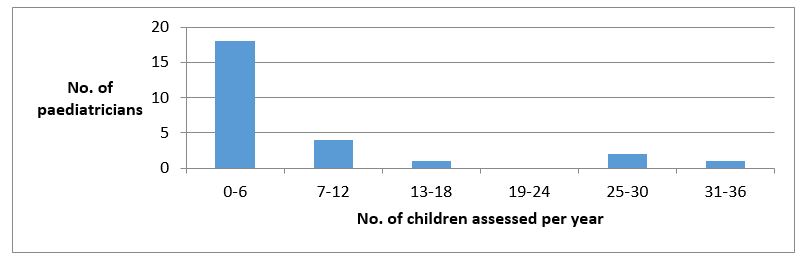
Figure 1: Number of paediatricians (Y-axis) reported assessing infants per year (X-axis)
Fourteen (42%) paediatricians see the child in a dedicated hearing (5/33) or developmental clinic (9/33), while only 24.2% (8/33) paediatricians continue to see them in a separate clinic. Only 75% of responders provide on-going follow up for their PCHL child after the initial assessment. Only two ( 3.6%) of the paediatricians participate in a regional support network but the majority (92.9%) expressed a desire to join one, provided they had dedicated time to do so. Regrettably only a third (11/33) of paediatricians surveyed reported an interest in on-going involvement in the service.
Two protocols are predominantly used in Ireland to guide the investigation of a child identified with PCHL, an unpublished Irish guideline, developed by a clinical geneticist and paediatrician[xi] a number of years ago and the British Association of Audiovestibular Physicians (BAAP) guidelines 6. Twenty-four (73%) paediatricians reported referring to a protocol, with the majority (20/24) of those using the BAAP guideline and 9/24 also referring to the Irish guideline. There was a consensus that if an agreed national protocol were developed it would be used by 29/33 (89.3%).
The BAAP guideline recommends that all children with PCHL should have an MRI IAM and brain, as there is a high diagnostic yield of between 30-40%7. Of 28 replies to this question only 16/28 (57%) reported ordering MRI regularly. Half of those who order MRI can access it within the window for natural sleep; therefore most children require sedation, often a general anaesthetic, to facilitate the scan.
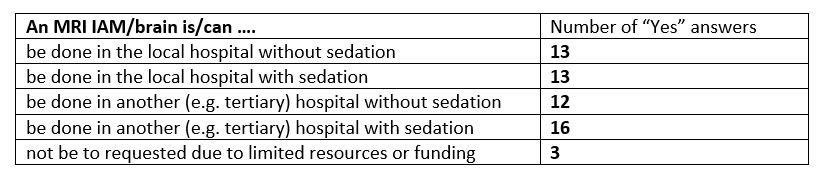
Table 2: MRI AIM and Brain requests by paediatricians
The BAAP guidelines states: “20-60% of children with PCHL have ophthalmic abnormalities which can remain undetected and impact on the child’s communication” 6. Twenty-four (73%) paediatricians routinely refer for ophthalmology assessment. In our survey, the community ophthalmologist was the most commonly reported ophthalmological specialist to provide the ophthalmology assessment (see table 3), this is consistent with the recommendations of the National Model of Care for Paediatric Healthcare[xii] .
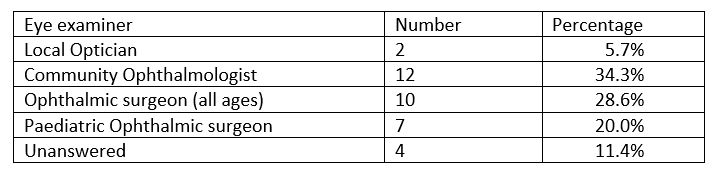
Table 3: Ophthalmological requests by paediatricians
Discussion
Universal neonatal hearing screening (UNHS) is well established in Ireland. The screening programme is appropriately funded and resourced with specially trained screeners and audiologists. Uniform protocols, structured quality assurance and ICT systems supported by regional and national governance structures have allowed the provision of an equitable service to all babies nationally. It is recognised that screening protocols should also include access to on-going diagnosis and treatment[xiii]. A 2008 WHO document recommended that screening programmes “should integrate education, testing, clinical services and programme management”[xiv]. This survey indicates significant deficits in the availability of appropriately trained paediatricians to assess and manage infants in a timely fashion, which is in contrast to the equity and quality of the UNHS screening component. Identified gaps include inadequate training, deficiencies in infrastructural local support and limited access to tertiary support i.e. genetics, ENT and infectious diseases services. The absence of an agreed nationally endorsed guideline and variation in access to radiology, genetics, and ophthalmology also impact on the ability to appropriately assess identified infants.
It is acknowledged that this survey relies on a questionnaire with obvious inherent limitations of accuracy. No consistent national activity levels or quality of service audits were routinely collected at the time of this survey in 2016. On foot of earlier informal discussions and feedback of this survey to those surveyed, local audits have been performed supporting the findings in this survey[xv].
The current medical management of infants and children with PCHL in Ireland is inadequate and puts our most vulnerable at risk. As a result of this audit, an integrated care pathway for children with PCHL is in development[xvi]. It is anticipated that in the future, regionalisation of paediatric services will allow cohorting of cases to facilitate the development of local expertise and the development of networks to allow discussion and tertiary review of challenging cases. The development of a more effective regional approach is proposed which would be provided by adequately trained, resourced and locally and regionally supported paediatricians with expertise in child development, knowledge of disability service structures and all relevant aspects of the aetiological assessment of children with permanent hearing loss using a nationally agreed standardised assessment process.
Future development will also require development of facilities to allow access to investigations such as MRI, ophthalmology, genetics and infectious diseases. A proposal to screen for cCMV at the point of failed new-born hearing screening is in development. A national governance and audit structure is required to ensure high standards and equitable services are realised and maintained, closely linked with the UNHS.
Conflict of Interest
The authors report that they have no conflicts of interest to declare.
Correspondence:
Dr Joanne Balfe, Department of Neurodisability and Developmental Paediatrics,
Tallaght University Hospital,
Dublin 24
E-mail: [email protected]
References
1. MacArdle, B. and M. Bitner-Glindzicz, Investigation of the child with permanent hearing impairment. Archives of disease in childhood - Education & Practice edition, 2010. 95(1): p. 14-23.
2. Sirimanna, T. and L. Batchelor, Role of the doctor in the UNHS team. Endorsed by Executive Committees of BAAP (British Association of AudioVestibular Physicians) and BAPA (British Association of Paediatricians in Audiology), July 2008.
3. Universal Newborn Hearing Screening Programme HSE. National Governance Document for the Health Services Executive. 2014, HSE.
4. National Universal Newborn Hearing Screening Referral Report 2016. eSP database, Northgate. HSE and Lesley Burn Consultancy. Report on the external quality assurance review of the universal hearing screening programme in Dublin North East and Dublin mid Leinster: recommendation action plan, HSE, Editor. 2015.
5. British Association of Audiovestibular Physicians. Guidelines for aetiological investigations into unilateral/bilateral permanent childhood hearing impairment. April 2015; Available from: http://www.baap.org.uk/Resources/Documents,GuidelinesClinicalStandards.aspx
6. England NHS Newborn Screening Program standards, developed internally based on a number of other UK standards and guidelines issued by NDCS, BAAP, BSA/BAA. 2015
7. BAAP/BAPA Guidelines for investigating infants with congenital hearing loss identified through the newborn hearing screen: Best practice guidelines. 2008 Available from http://www.bapa.uk.com/userfiles/Congenital%20Hearing%20Loss%20Investigation%20in%20the%20Newborn%20BAAP%20BAPA%20Guideline%202008(1).pdf
8. Marsico, C and Kimberlin D. Congenital Cytomegalovirus infection: advances and challenges in diagnosis, prevention and treatment. Italian Journal of Pediatrics 2017 43:38
9. British Association of Audiovestibular Physicians Clinical Standards: setting standards to improve care for patients with hearing and balance disorders 2011
10. Kyne L. Personal Correspondence
11. Health Service Executive. A National Model of Care for Paediatric Healthcare Services in Ireland. Chapter 37: Paediatric Ophthalmology. 2017.
12. Wilson, J.M.G. and G. Jungner, Principles and practice of screening for disease. Public Health Paper 34, World Health Organization, 1968. 34.
13. Andermann, A, Blancquaert I, Beauchamps S & Dery V Revisiting Wilson and Jungner in the genomic age: a review of screening criteria over the past 40 years. Bull World Health Organisation, 2008. 86(4): p. 317-9.
14. Smith A, O’Connor A, Hennessy S, O’Sullivan P.G. , Gibson, L. Permanent Childhood Hearing Impairment: Aetiological Evaluation of Infants identified through the Irish Newborn Hearing Screening Programme. IMJ 2018 Dec
15. Health Service Executive. Annual report and Financial Statement 2017, page 28. https://www.hse.ie/eng/services/publications/corporate/annual-report-and-financial-statements-2017.pdf accessed 6 July 2018
P804
