Obstetric Anal Sphincter Injuries: A Survey of Clinical Practice and Education among Obstetricians and Gynaecologists in Ireland
M. Abdelrahman1, M. Geary1, M. Eogan1
1Rotunda Hospital, Dept. of Obstetrics and Gynaecology, Parnell Square, Dublin 1
Abstract
This paper summarises results of a survey of obstetricians in Ireland regarding their technique, management, and education on episiotomy and Obstetric Anal Sphincter Injury (OASIS). An anonymous survey was emailed to all obstetricians and gynaecologists in Ireland, including trainees between January and September 2017. The response rate was 45% (155/343) with 111 out of 144 (77%) reported clinical experience as part of their training and 92 (64%) attended an OASIS workshop or classroom teaching. The majority prescribe antibiotics and laxatives post-op, request physiotherapy review and follow-up patients in outpatient settings.
We identified that most specialists and trainees practice within guidelines, but some recognise a need for further teaching and exposure to these types of injuries. These results will direct future curriculum and optimise ongoing training for trainees, unify service provision and contribute to patient safety.
Introduction
Obstetric Anal Sphincter Injuries (OASIS) encompass both third and fourth degree perineal tears, which occur in approximately 2% of vaginal births in Ireland.1 Postnatally, the prevalence of anal incontinence is higher among women with OASIS (8-17%) compared to women without (3-8%).2-5 While chronic postpartum morbidities such as anal incontinence may not be life threatening, they can significantly affect quality of life, so prevention of such morbidities is always a priority. With prompt recognition and repair, long-term sequelae are reduced, and 60-80% are asymptomatic at 12 months follow up.6-9 Unfortunately, primary prevention of OASIS is challenging, as many of the risk factors for injury such as primiparity, occipito-posterior position, birthweight over 4kg and instrumental delivery are frequently encountered in births that are not complicated by OASIS, and thus are not entirely avoidable. Nevertheless, appropriate use and angle of episiotomy as well as prudent use of perineal support during delivery are effective interventions that reduce OASIS.6,10
Initiatives that may reduce OASIS rates include provision of care bundles, such as the recent implementation of the OASI care bundle in the UK— which aims to increase the use of standardised prevention practices, including perineal support during delivery and appropriate use of episiotomy.11 Postnatal care is also important, including provision of antibiotics, laxatives and appropriate follow up including physiotherapy.
Studies have been performed to assess trainees’ and specialists’ knowledge and training with regard to management of OASIS. A Canadian survey identified that many obstetricians did not follow evidence-based practice in terms of the use of prophylactic antibiotics, postoperative management of bowel activity, and recommendations for pelvic physiotherapy.12 Another survey of a small number of trainees concluded that there is a need to improve the training of residents in the management of perineal injuries during delivery and postpartum.13 These studies concluded that the implementation of a structured “hands-on” workshop to educate health care professionals regarding current evidence and development of a pro forma “tick box” and standardised protocol, would further reduce any barriers that may deter adoption of these evidence-based techniques for management of these injuries.12,13
Methods
A 20 question electronic survey was emailed to all obstetricians and gynaecologists in Ireland, including trainees at all levels between January and September 2017. It was created using GoogleForms and was adapted from one previously distributed in Canada.12 This was an anonymous survey with no identifying information collected from participants. No incentives or disincentives were offered to complete it. Results were analysed using the Pearson’s Chi-square, Mann-Whitney-U, and Fisher’s exact tests on SPSS where appropriate.
Results
Context
The survey response rate was 45% (155/343, N=155), 117 (75%) responses were from Non Consultant Hospital Doctors (NCHDs) followed by 38 responses (25%) from consultants. Of the NCHDs, 93 (79%) were Higher Specialist Trainees (HSTs) and Basic Specialist Trainees (BSTs). The majority, 94 (61%), of respondents worked in units with more than 6000 births annually while 46 (30%) worked in units between 2000 and 6000 births annually, 13 (8%) worked in units with less than 2000 births per year and 2 (1%) were unsure of their unit’s birth rates.
Episiotomy repair and techniques
Out of 155, 102 respondents (66%) reported that the most common method of episiotomy was right mediolateral followed by 18% right lateral (28/155). Seventy-one respondents (46%) stated they use specially designed scissors with a vertical guide limb (eg. Episcissors™) to cut episiotomies, 44 (28%) stated that these were not available in their maternity unit and 14 (9%) preferred not to use them. One hundred and forty four respondents (93%) repair episiotomies, with only 11 (7%) stating they do not; the main reasons being that the midwifery team repair them or they are in a gynaecology post at present, with minimal/no obstetric practice— these respondents did not complete any further questions in survey.
OASIS repair training and management
In relation to training, 111 out of 144 (77%) of those who answered the rest of the questionnaire stated that part of their learning regarding OASIS diagnosis and repair was accrued through clinical experience, but 92 (64%) also reported attending a workshop or didactic classroom teaching and 36 (25%) engaged in an online course. In relation to diagnosing OASIS, 58/144 (40%) identified as being ‘1- very confident’ on a scale of 1-5, with almost 10/144 (7%) scoring ‘5- not confident at all'.
In total, 105/144 of respondents (73%) repair third and fourth degree tears. However, 39 respondents (27%) stated they do not repair third or fourth degree tears. Of those that do not repair OASIS, 18 (46%) stated they did not receive training and 12 (30%) felt they were not competent despite receiving training for such. Of those that repair OASIS, approximately 45% (47/105) estimate that they repair less than 5 cases annually, 38% (40/105) repair 5-10 cases, 7% (8/105) repair 10-15 cases and 10% (10/105) repair more than 15 cases annually, these doctors all work in units with more than 6000 births annually. Eighty-six (82%) perform OASIS repair in the operating theatre, 18 (17%) choose either the labour ward or theatre depending on circumstances and 1 (1%) prefer repairing it in the labour ward.
Ninety-six respondents (91%) would choose to repair a third degree tear under regional anaesthesia, but 5% also answered that they would use local, pudendal block or regional anaesthesia, 3% would repair OASIS under regional or general anaesthesia, and less than 1% would prefer general anaesthesia only. Sixety-one respondents (58%) would choose a 3-0 Polydioxanone suture for the repair of the external anal sphincter followed by 34% that would use 2-0 Polydioxanone and 7% would prefer 1-0 or 2-0 Polyglactin 910. One person (<1%) stated ‘unknown’ for suture material preferred.
For the repair of a fourth degree tear, 88 respondents (84%) would prefer regional anaesthesia, 6% would prefer regional or general anaesthesia, 2% would choose either local, pudendal block or regional anaesthesia, and less than 1% would prefer general anaesthesia. Eight respondents (7%) did not know what type of anaesthesia they preferred as they have never repaired a 4th degree tear. Similarly, 81 respondents (77%) use 3-0 Polyglactin 910 suture for repair of rectal mucosa, 8% use 4-0 polyglactin, 8% use 3-0 or 4-0 polydiaxanone, less than 1% use 2-0 Polyglactin 910 but 7 respondents (6.6%) had never repaired a fourth degree tear therefore they did not know what type of anaesthesia they preferred or suture material for the rectal mucosa.
Post operative management
Seventy- six respondents (72%) leave an indwelling catheter in-situ and the majority, 96/105 (91%), also prescribe prophylactic antibiotics and laxatives postnatally. With regards to physiotherapy, 83 respondents (79%) stated they request review while in hospital, 12 (11%) would request review between 2-6 weeks postnatally and 6 (5.7%) stated they would be reviewed by physiotherapy more than 6 weeks postnatally. Only one participant (<1%) stated they would not request physiotherapy.
Follow-up care
Forty-seven respondents (45%) disclosed that patients are followed up in a hospital based gynaecology/postnatal clinic with 51% (54/105) reviewed in a specialist perineal clinic. Two respondents (1.8%) stated their patients would receive outpatients physiotherapy review only, and one person would refer them for primary care (GP) follow up.
Training and grade of experience and their impact on results
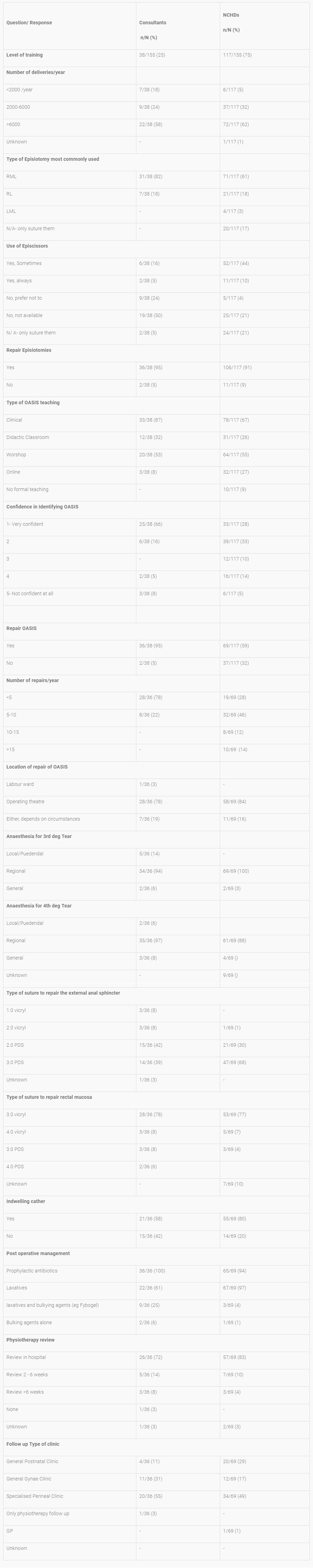
Results were further analysed to broadly assess the impact of types of training and grade of experience on skills, confidence and management (See tables 1 and 2 below). Ninety-two respondents (64%) reported participation in a workshop and/or didactic classroom teaching on OASIS diagnosis and repair. Fifty-two respondents (36%) reported having only clinical experience and/or attending an online course and/or having no formal teaching regarding OASIS management. When comparing confidence in diagnosing and repairing an OASIS, 79% of those who attended a workshop/classroom training scored 1- 2 on the scale for confidence vs. 60% in the clinical/online/no formal training group (p=0.106). Furthermore, 82% of consultants scored 1-2 compared to 62% of NCHDs (p<0.001). There was no statistically significant difference between training groups or grades of experience in relation to the location, anaesthesia or technique preferred when repairing OASIS. Similarly, the results were alike when comparing post-operative management and follow up care.
Table 1: Survey response rates according to training group
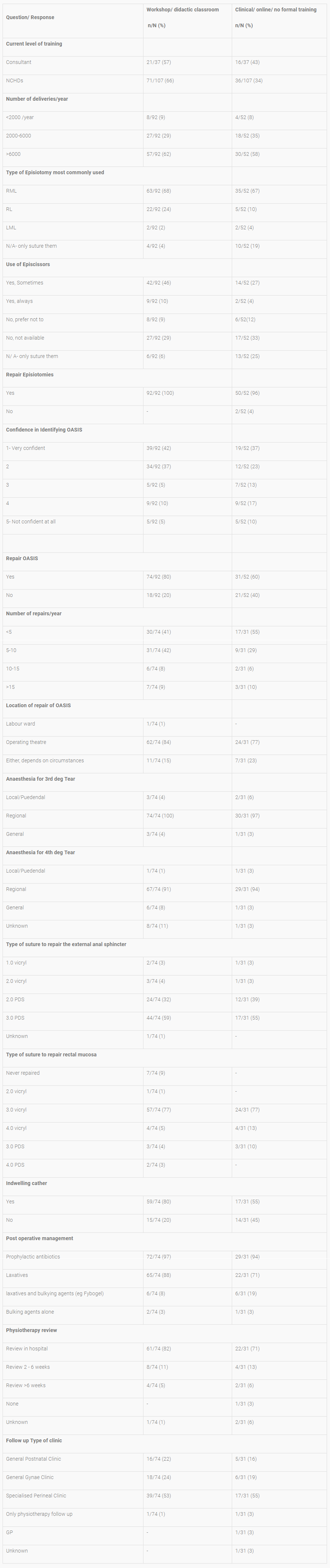
Table 2: Survey response rates according to grade of experience
Discussion
Similar to all surveys, the limitations of our study include a response rate of 45%, not representing the opinions of all obstetricians in Ireland, and with unequal responses from different grades of experience and training possibly contributing to the lack of statistical significance when comparing results. However, this questionnaire was anonymous, disseminated widely and our results demonstrate that the majority of respondents demonstrated awareness of recommended best practice and are compliant with Institute of Obstetricians and Gynaecologists (IOG)/ RCPI and RCOG guidelines for the management of OASIS.6,14 While the results show that clinical seniority may enhance confidence in diagnosing and repairing OASIS, it is very reassuring that all other aspects of care are excellent – even in those who have not attended formal training.
With regards to primary prevention practices, it is important to ensure that practitioners are taught to cut episiotomies at the appropriate angle. Simulation models have identified that only 15% of doctors and midwives cut episiotomies between 58 and 62 degrees from the midline.6,15,16 Episcissors™ are reusable scissors that facilitate performing episiotomies at a 60 degree angle from the midline with the aim of reducing incidence of anal sphincter injuries.17
Some studies suggest that structured teaching and hands-on workshops are advantageous interventions that increase trainees’ confidence levels in classifying, identifying and managing OASIS.18-20 While this study identified that trained doctors (consultants) were more confident in diagnosing OASIS (p<0.001), attending a workshop/classroom teaching was not associated with an increase in confidence (p=0.106). Workshop/classroom training may however improve some aspects such as physiotherapy review requests prior to discharge (p<0.0001).
In relation to the use of a stool-bulking agent (e.g. Fybogel) in addition to a laxative in the immediate postnatal period, this may increase incontinence without improving patients’ pain scores or pain related to the first bowel motion.21 It is noted in our study more participants in the clinical/online/no formal training group would prescribe laxatives with a bulking agent than the classroom/workshop group (22% vs 9%, p=0.067) as would more consultants versus NCHDs (29% vs 5%, p< 0.001).
At present, all trainees are required to attend a practical surgical skills workshop early in their training. These sessions should include episiotomy cutting and repair practice models . A hands-on OASIS workshop involving simulation should also be offered. This would allow dissemination of guidelines and afford trainees the opportunity to learn, practice and be assessed on their repair techniques.
Similar to recent investment in the NHS, we would encourage all maternity units to obtain Episcissors™ to encourage its staff, particularly junior doctors and midwives, to perform episiotomies when indicated and to ensure that episiotomies are cut at safe angles to reduce the risk of OASIS. With the introduction of the electronic maternal and newborn clinical management system in Ireland (MN-CMS), there is an opportunity to provide an electronic OASIS care bundle and a pro-forma for OASIS repairs to ensure sustained compliance with clinical guidelines.
Conflict of Interest
The authors declare that there is no conflict of interest.
Acknowledgements
We would like to thank the Institute of Obstetricians and Gynaecologists, Royal College of Physicians in Ireland for their assistance in the distribution of the survey as well as Colin Kirkham for his assistance with statistical analysis of the data.
Corresponding Author
Dr. M Abdelrahman,
Rotunda Hospital,
Dept of Obstetrics and Gynaecology,
Parnell Square, Dublin 1
Email: [email protected]
References
1. Irish Maternity Indicator System National Report 2015. HSE Clinical Programme in Obstetrics and Gynaecology. August 2016. Available from: https://www.hse.ie/eng/services/publications/NursingMidwifery%20Services/Irish-Maternity-Indicator-System-National-Report-2015.pdf
2. Laine K, Skjeldestad FE, Sanda B, Horne H, Spydslaug A, Staff AC. Prevalence and risk fac-tors for anal incontinence after obstetric anal sphincter rupture. Acta Obstet Gynecol Scand. 2011;90(4):319-24.
3. Guise JM, Morris C, Osterweil P, Li H, Rosenberg D, Greenlick M. Incidence of fecal inconti-nence after childbirth. Obstet Gynecol. 2007. 109:281-288.
4. Eason E, Labrecque M, Marcoux S, Mondor M. Anal incontinence after childbirth. CMAJ. 2002;166(3):326-330.
5. Borello-France D, Burgio KL, Richter HE, Zyczynski H, Fitzgerald MP, Whitehead W, Fine P, Nygaard I, Handa V, Visco AG, Weber A, Brown MB. Fecal and urinary incontinence in pri-miparous women. Obstet Gynecol. 2006;108(4):863-872.
6. Royal College of Obstetricians and Gynaecologists. Green-top guideline No. 29. The Manage-ment of Third and Fourth-Degree Perineal Tears. 2015. Available from: https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg29.
7. Eogan M, O'herlihy C. Diagnosis and management of obstetric anal sphincter injury. Curr Opin Obstet Gynecol. 2006;18(2):141-146.
8. Mahony R, Behan M, Daly L, Kirwan C, O'Herlihy C, O'Connell PR. Internal anal sphincter de-fect influences continence outcome following obstetric anal sphincter injury. Am J Obstet Gy-necol. 2007;196(3):217.
9. Roos AM, Thakar R, Sultan AH. Outcome of primary repair of obstetric anal sphincter injuries (OASIS): does the grade of tear matter? Ultrasound Obstet Gynecol. 2010;36(3):368-374.
10. Laine K, Pirhonen T, Rolland R, Pirhonen J. Decreasing the incidence of anal sphincter tears during delivery. Obstet Gynecol. 2008;111:1053e7.
11. The OASI care bundle project. NHS. Available from: https://www.rcog.org.uk/OASICareBundle.
12. Menzies R, Leung M, Chandrasekaran N, Lausman A, Geary M. Episiotomy Technique and Management of Anal Sphincter Tears:A Survey of Clinical Practice and Education. J Obstet Gynaecol Can. 2016;38(12):1091e1099
13. Cornet A, Porta O, Piñeiro L, Ferriols E, Gich I, Calaf J. Management of Obstetric Perineal Tears: Do Obstetrics and Gynaecology Residents Receive Adequate Training? Results of an Anonymous Survey. Obstetrics and Gynecology International. 2012;2012:316983.
14. Royal College of Physicians in Ireland. Clinical Practice Guideline No. 8: Management of Ob-stetric Anal Sphincter Injury. 2012. Available from:https://www.rcpi.ie/faculties/obstetricians-and-gynaecologists/national-clinical-guidelines-in-obstetrics-and-gynaecology.
15. Naidu M, Kapoor DS, Evans S, Vinayakarao L, Thakar R, Sultan AH.Cutting an episiotomy at 60 degrees: how good are we? Int Urogynecol J. 2015;26(6):813-6.
16. Kalis V, Landsmanova J, Bednarova B, Karbanova J, Laine K, Rokyta Z. Evaluation of the incision angle of mediolateral episiotomy at 60 degrees. International Journal of Gynaecology and Obstetrics. 2011;112: 220–4.
17. NICE Medtech innovation briefing. Episcissors-60 for guided mediolateral episiotomy. July 2015. Available from: https://www.nice.org.uk/advice/mib33.
18. Andrews V, Thakar R, Sultan AH. Outcome of obstetric anal sphincter injuries (OASIS)—role of structured management. Int Urogynecol J. 2009;20: 973.
19. Andrews V, Thakar R, Sultan AH. Structured hands-on training in repair of obstetric anal sphincter injuries (OASIS): an audit of clinical practice. Int Urogynecol J Pelvic Floor Dysfunct 2009;20:193e9.
20. Emmanuelli V, Lucot JP, Closset E, Cosson M, Deruelle P. Development and assessment of a workshop on repair of third and fourth degree obstetric tears. J Gynecol Obstet Biol Reprod. 2013;42:184e90.
21. Eogan, M., Daly, L., Behan, M., O’Connell, P. and O’Herlihy, C. Randomised clinical trial of a laxative alone versus a laxative and a bulking agent after primary repair of obstetric anal sphincter injury. BJOG. 2007;114: 736–740.
P852
