Outcomes of a Community-Based Paediatric Weight Management Programme in an Irish Midlands Setting
AE Bennett1, C Johnston Molloy2, C Glennon-Slattery2, D Loane3
1 Department of Clinical Medicine, School of Medicine, Trinity Centre for Health Sciences, St. James’ Hospital Campus, Dublin 8, Ireland
2 Community Nutrition and Dietetic Service, Health Service Executive, CHO Area 8, Primary Care Unit, St Loman’s Hospital, Mullingar, County Westmeath, Ireland
3 Community Nutrition and Dietetic Service, Health Service Executive, CHO Area 8, Primary Care Centre, Connolly Street, Mountmellick, County Laois, Ireland
Abstract
Ongoing investigation is needed into feasible approaches which reduce excess weight in childhood. This study aimed to assess the effectiveness of an adapted version of the Scottish Childhood Overweight Treatment Trial (SCOTT) in an Irish primary care setting. Families were offered monthly dietitian-led sessions for six months. These sessions targeted dietary habits, family meals, screen time and exercise. Of the 95 children (mean age 7.6 years) referred, 90.5% (n86) were obese and 9.5% (n9) were overweight. Fifty-one (53.7%) families opted into the programme from referral, and 18 completed the programme (64.7% attrition). Statistically significant reductions in body mass index (BMI) were observed between sessions one and six (25.7±4.2kg/m2 and 25.3±4.8kg/m2, respectively, p<0.01). BMI z-score modestly decreased by 0.2 (p=0.01). Despite these reductions, issues with programme referral, attrition and long-term effectiveness were evident. Further investigation into strategies which reduce paediatric overweight is warranted.
Introduction
Obesity is a recognised complex and chronic condition with serious physical, social and psychological implications1. The management of childhood obesity has proven to be an exceptionally challenging task with no clear solution to date2, as evidenced by the slow and inconsistent progress in tackling this issue3. Recent Irish literature4,5 has highlighted the importance of translating weight management programmes which have proved effective in clinical studies, into effective programmes within the primary care setting. However, the results of published weight management programmes have been inconsistent6,7,8,9,10 to date. The innumerable factors which comprise an obesogenic environment make it difficult to identify the combination of factors which, if targeted, would provide a feasible and effective long-term solution to childhood obesity. However, it is generally accepted that intervention effectiveness is favoured by the inclusion of components such as: behaviour change techniques11,12, parental involvement9,10,13, dietary modification6,8,9, family meals8, reduced screen time8,10, and increased exercise6,8,10.
This study aimed to assess the clinical effectiveness of a paediatric weight management programme8 which had been published as a randomised controlled trial, once it was adapted for the primary care setting by the Community Nutrition and Dietetic Service (CNDS) in Community Health Organisation (CHO) Area 8, Ireland.
Methods
Ethical approval was granted by the Research Ethics Committee of the Health Service Executive Midlands Area. Parental consent and child assent were obtained prior to participation. Children aged 4-13 years who did not have an organic cause to their excess weight were eligible to avail of the adapted programme. The weight management programme implemented in this study was adapted from the Scottish Childhood Overweight Treatment Trial (SCOTT)8. The SCOTT programme, which included eight family-centred appointments with a dietitian over six consecutive months, was adapted and implemented by the CNDS in CHO Area 8 (Midlands). When available resources and long-term feasibility were considered, a reduction from eight to six appointments over six months was necessary. Programme tools were also modified to reflect Irish recommendations on healthy eating. The family-centred approach and behavioural change techniques used in the original programme were maintained.
The programme aimed to address childhood overweight by empowering parents to take responsibility for their child’s increasing weight. This approach sought to enable parents to embed healthier practices in their family’s daily environment, and therefore in the environment of the child of interest. Practices such as dietary intake, family meals, screen time and exercise were targeted. Since parents are most often the gatekeepers to changing the dietary and lifestyle habits of a child, the child of interest attended only appointments two and six with their parent. The remaining four appointments involved only the dietitian and parent. Cognitive behavioural therapy (CBT) techniques were used to enhance parental motivation to introduce positive lifestyle changes amongst their family. All dietitians involved had received formal training in Dymphna Pearson’s validated Behaviour Change Training model. The CBT techniques used included: goal-setting; managing barriers; identifying suitable rewards and supports; initiating healthy self-monitoring; and preventing relapse. Therefore, evidence-based best practice underpinned the programme8.
All data were collected by community dietitians. Anthropometric data (weight, height and body mass index (BMI)) on the child of interest, and on parents and siblings in attendance, were collected at appointments two and six. Data on behaviours such as: family meals (never, sometimes or always); screen time (minutes/day); and physical activity (<60 minutes/day versus >60 minutes/day) were also collected. Data were inputted into SPSS version 22.0 and presented descriptively using frequencies, means and standard deviations. Comparisons were made between anthropometric measurements using one-sample t-tests.
Results
Characteristics of children referred
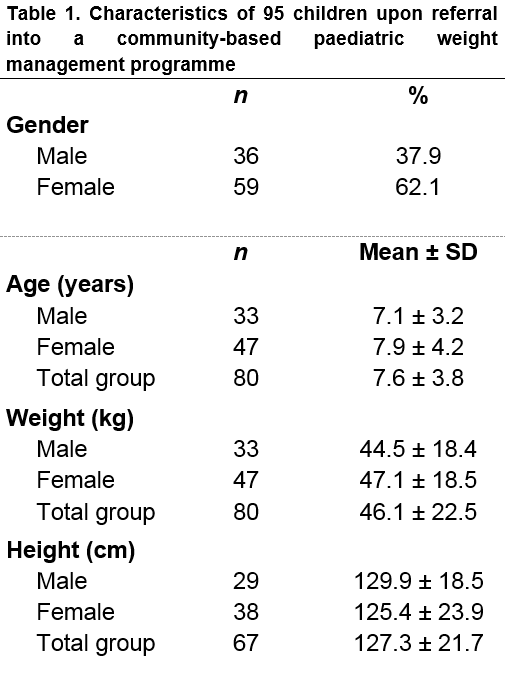
Of the 95 children referred, most (62.1%, n59) were female and had a mean age of 7.6±3.8 years (Table 1). Of those referred, 90.5% (n86) were obese and 9.5% (n9) were overweight.
Opt-in rates
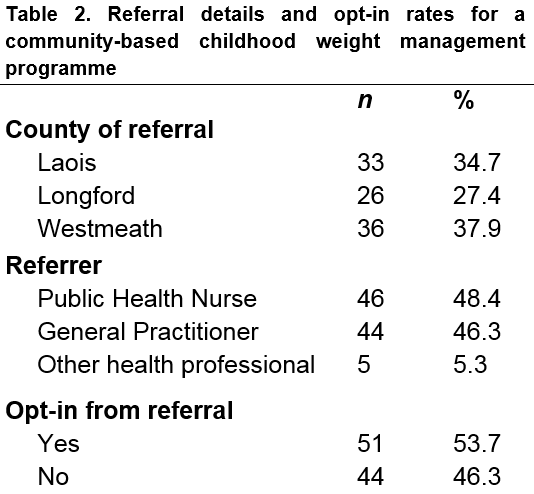
There was a reasonably even distribution of referrals across Laois, Longford and Westmeath (Table 2). Public health nurses and general practitioners referred 48.4% and 46.3% of children, respectively. However, although all guardians were aware of, and agreed to, the referral, almost half (46.3%, n44) did not proceed with making an appointment when offered one by the service.
Attendance and attrition
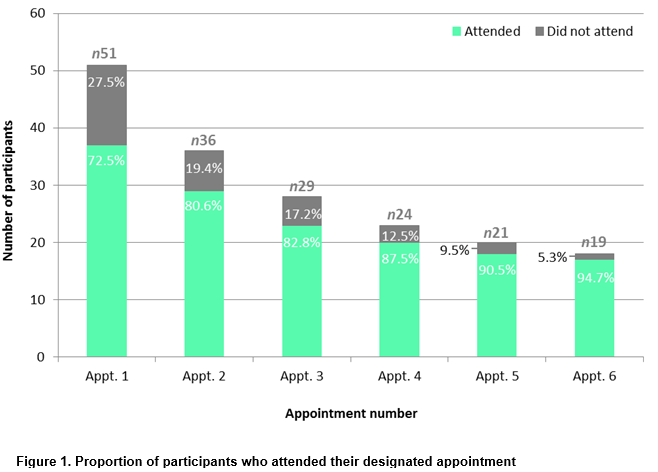
The rates of attendance and attrition amongst those who opted into the programme are shown in Figure 1. Once a parent did not attend an appointment, their child was discharged, as indicated by the decreasing sample size over time. Of the 51 parents who made an appointment upon referral, over a quarter (27.5%, n14) did not attend their first appointment. Therefore, of the 95 families referred, only 37 (38.9%) attended at least one appointment with a dietitian.
Of the 95 children referred, 51 parents were due to attend appointment one, and 19 were due to attend appointment six; however, 37 parents actually attended appointment one and 18 attended appointment six, resulting in 64.7% attrition over the course of the programme. Although high rates of attrition were observed at the first appointment, rates consistently decreased thereafter (Figure 1). Child gender and BMI did not significantly differ between those who did and did not attend appointments.
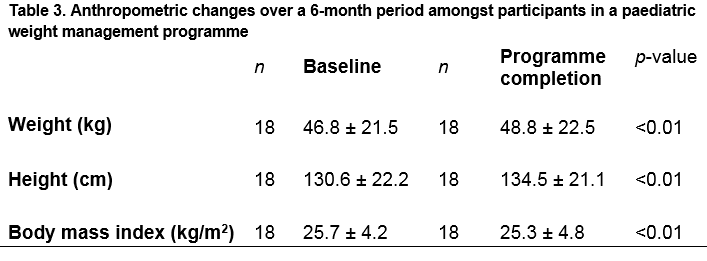
Anthropometric changes
The anthropometric measures obtained on children who attended appointments two and six (n18) are compared in Table 3. When compared to the mean BMI at baseline, the mean BMI after the programme was significantly (p<0.01) lower, as was the BMI z-score (p=0.01), which decreased by 0.2 between baseline and the end of the programme.
Challenges observed
Challenges recorded by dietitians included inappropriate weight-related language being used by parents in the presence of children and difficulties getting all family members to support the programme.
Discussion
This study assessed the effectiveness of an evidence-based childhood obesity programme which was adapted for an Irish primary care setting. Although programme completers achieved statistically significant reductions in their BMI z-score, the findings highlighted considerable challenges in terms of referral, attrition and long-term clinically significant weight loss.
Of those referred, almost half of parents did not make an appointment for their child to participate in the programme, despite agreeing to a referral being made. The manner in which health professionals communicate with parents over their plans to refer a child to a weight management programme must be considered5,14. Over half of parents underestimate their child’s weight15, and parents of overweight and obese children are known to distrust the assessment of health professionals, often not perceiving excess weight as a condition which requires immediate attention14,16.
Inadequate parental motivation to participate in a paediatric weight management programme is detrimental to programme effectiveness7,13,14. It has been recommended5 that health professionals receive consultation skills training to help them to tactfully emphasise the seriousness of excess weight in childhood whilst maintaining a positive rapport with parents. Parents may be concerned about the potential psychological (e.g. reinforcing the weight problem), educational (e.g. taking time from school to attend) or financial (e.g. travel costs) implications of committing to a programme14,16, and therefore it is important that any such concerns are anticipated and addressed from the outset, as part of the referral process.
Once a parent engages in a programme with their child, they must be encouraged to participate in a manner which encompasses the whole family and addresses the eating and lifestyle behaviours of all family members17,18. This collective effort is necessary to promote better family support, and therefore to potentially decrease the likelihood of attrition. The attrition rate for this programme, at 64.7%, was high. Attrition rates ranging from 10% to 73% for paediatric weight management programmes have been reported in the literature18, and it is known that such programmes often suffer from this particular concern19.
Programme attrition is a multifaceted problem, complicated by participant characteristics, programme characteristics and logistical issues18,19. Participant characteristics are reportedly weak predictors of engagement in paediatric weight management programmes19, and therefore greater emphasis should be placed on programme characteristics when trying to reduce attrition. Several studies have investigated strategies which could reduce rates of attrition18,19, and such strategies include: appropriate reminders on the importance of participation18; mandatory and meaningful parental involvement7; setting realistic expectations for weight loss14; programme delivery across the autumn and winter19; and online interactive tools to promote engagement between sessions20. Online interactive tools are showing particular promise in terms of modifying health behaviours20,21, since they are generally a feasible means of engaging with participants on a more frequent basis. Further investigation into the role of online tools in paediatric weight management programmes may provide valuable insights into effective strategies which reduce attrition.
However, logistical challenges, such as work and school obligations, travelling distances to clinic and competing family commitments, are also common contributors to attrition rates14,18. Logistical challenges are often outside the control of a service provider, and if these challenges are reported to be primarily responsible for attrition, identifying strategies to improve programme engagement can be difficult. Again, investigating the use of online technology may prove helpful in overcoming logistical challenges and increase the likelihood of favourable intervention outcomes.
Despite the challenges of referral and attrition, statistically significant weight loss was observed in this study. The reduction in BMI z-score is comparable to reductions reported by other programmes8,10,22,23, which is positive. However, the reductions observed were modest and the sample size was much reduced at the end of the programme, making it difficult to draw conclusions on its overall effectiveness. Follow-up at six months and one year post-completion would provide important insights into the long-term effectiveness of the programme7. Measuring long-term effectiveness is an essential part of justifying the significant cost and resource implications involved in reducing overweight in childhood. Therefore, although it can be tentatively concluded that the programme was modestly effective, further review and adaptation are undoubtedly needed.
Before concluding, the study strengths and limitations must be considered. The SCOTT programme8 is an evidence-based programme which was adapted to ensure that it was suitable for use in an Irish primary care setting. Despite reducing the number of appointments from eight to six appointments and adapting tools to suit an Irish context, all other elements of the programme remained largely the same, and statistically significant weight loss – slightly higher than that reported by the original programme7,8 – was observed. However, rates of attrition in this study were higher than those in the original programme, so completers in this study most likely represent a highly motivated sub-group; this is an important consideration when interpreting the weight loss observed. Overall, although further investigation is needed into approaches which encourage participation and reduce attrition, the adapted programme is not without potential. With further adaptation, it may yet prove to be a valuable tool in managing paediatric overweight in the community.
As the environment in which children are raised becomes increasingly obesogenic, further investigation into childhood overweight and obesity is paramount. This study is one of the first to adapt and evaluate an evidence-based paediatric weight management programme for use by a CNDS in Ireland. The findings, although not without promise, clearly indicate that further evidence-based work in this area is needed. However, even more importantly, the findings emphasise the elusiveness of a cure to the pervasive issue of excess weight in childhood, and highlight the need to focus our efforts on prevention, in order to better protect the long-term health and wellbeing of children.
Correspondence
Annemarie E. Bennett, Department of Clinical Medicine, School of Medicine, Trinity Centre for Health Sciences, St. James’ Hospital Campus, Dublin 8, Ireland
Email: [email protected]
Acknowledgement
This study was funded by Westmeath Community Development Ltd.
Conflict of interest
The authors have no conflict of interest to declare.
References
1. World Health Organisation. Report on the Commission on Ending Childhood Obesity. [Online] 2016; accessed from: www.who.int/end-childhood-obesity/publications/echo-report/en/.
2. Layte R, McCrory C. Growing Up in Ireland Study: overweight and obesity amongst 9-year-olds. [Online] 2009; accessed from: www.esri.ie/pubs/BKMNEXT211.pdf.
3. Department of Health. A healthy weight for Ireland: obesity policy and action plan. The Stationary Office. 2016; accessed from: http://health.gov.ie/wp-content/uploads/2016/09/A-Healthy-Weight-for-Ireland-Obesity-Policy-and-Action-Plan-2016-2025.pdf.
4. Dowd K, Murphy AM, Scully P, Letshwiti JB, O’Gorman C. The establishment of a pilot paediatric obesity clinic at the University Hospital, Limerick. Irish Medical Journal. 2015; 108: 278-280.
5. O’Shea B, Ladewig EL, Kelly A, Reulbach U, O’Dowd T. Weighing children; parents agree, but GPs conflicted. Archives of Disease in Childhood. 2014; 99: 543-545.
6. Reinehr T, Temmesfeld M, Kersting M, De Sousa G, Toschke AM. Four-year follow-up of children and adolescents participating in an obesity prevention program. International Journal of Obesity. 2007; 31: 1074-1077.
7. van der Kruk JJ, Kortekaas F, Lucas C, Jager-Wittenaar H. Obesity: a systematic review on parental involvement in long-term European childhood weight control interventions with a nutritional focus. Obesity Reviews. 2013; 14: 745-760.
8. Hughes AR, Stewart L, Chapple J, McColl JH, Donaldson MDC, Kelnar CJH, Zabihollah M, Ahmed F, Reilly JJ. Randomized controlled trial of a best-practice individualized behavioural program for treatment of childhood overweight: Scottish Childhood Overweight Treatment Trial (SCOTT). Pediatrics. 2008; 121: e539-e546.
9. Stewart L, Houghton J, Hughes AR, Pearson D, Reilly JJ. Dietetic management of pediatric overweight: development and description of a practical and evidence-based behavioural approach. Journal of the American Dietetic Association. 2005; 11: 1810-1815.
10. Korsten-Reck U, Kromeyer-Hauschild K, Wolfarth B, Dickhuth HH, Berg A. Freiburg Intervention Trial for Obese Children (FITOC): results of a clinical observation study. International Journal of Obesity. 2005; 29: 356-361.
11. Epstein LH, Roemmich JN, Raynor HA. Behavioral therapy in the treatment of pediatric obesity. Pediatric Clinics of North America. 2001; 48: 981-993.
12. van den Akker ELT, Puiman PJ, Groen M, Timman R, Jongejan MTM, Trijsburg W. A cognitive behavioral therapy program for overweight children. Journal of Pediatrics. 2007; 72: 465-472.
13. Hingle MD, O’Connor TM, Dave JM, Baranowski T. Parental involvement in interventions to improve child dietary intake: a systematic review. Preventative Medicine. 2010; 51: 103-111.
14. Perez A, Holt N, Gokiert R, Chanoine J-P, Legault L, Morrison K, Sharma A, Ball G. Why don’t families initiate treatment? A qualitative multicentre study investigating parents’ reasons for declining paediatric weight management. Child Health. 2015; 20: 179-184.
15. Lundahl A, Kidwell KM, Nelson TD. Parental underestimates of child weight: a meta-analysis. Pediatrics. 2014; 133: e689-e703.
16. Coppock JH, Ridolfi DR, Hayes JF, St Paul M, Wilfley DE. Current approaches to the management of pediatric overweight and obesity. Current Treatment Options in Cardiovascular Medicine. 2014; 16: 343-360.
17. Tremblay M, Perez AJ, Rasquinha AM, Avis JL, Morrison KM, Chanoine JP, Legault L, Holt NL, Gokiert R, Sharma AM, Ball GD. Recommendations from parents to improve health services for managing pediatric obesity in Canada. Academic Pediatrics. 2016; 16: 587-593.
18. Skelton JA, Martin S, Irby MB. Satisfaction and attrition in paediatric weight management. Clinical Obesity. 2016; 6: 143-153.
19. Nobles J, Griffiths C, Pringle A, Gately P. Design programmes to maximise participant engagement: a predictive study of programme and participant characteristics associated with engagement in paediatric weight management. International Journal of Behavioral Nutrition and Physical Activity. 2016; 13: 76-86.
20. Berkovsky S, Hendrie G, Freyne J, Noakes M, Usic K. HealthierU Portal for supporting behaviour change and diet programs. Studies in Health Technology and Informatics. 2015; 214: 15-21.
21. Lau Y, Htun TP, Tam WSW, Klainin-Yobas P. Efficacy of e-technologies in improving breastfeeding outcomes among peri-natal women: a meta-analysis. Maternal and Child Nutrition. 2016; 12: 381-401.
22. Kalavainen MP, Korppi MO, Nuutinen OM. Clinical efficacy of group-based treatment for childhood obesity compared with routinely given individual counseling. International Journal of Obesity. 2007; 31: 1500-1508.
23. Robertson W, Friede T, Blissett J, Rudolf MC, Wallis M, Stewart-Brown S. Pilot of ‘Families for Health’: community-based family intervention for obesity. Archives of Disease in Childhood. 2008; 93: 921-926.
P689