Oxygen Therapy in Ireland: A Nationwide Review of Delivery, Monitoring and Cost Implications
C. O’Donnell1, P. Davis2, T. McDonnell1
1. St. Vincent’s University Hospital
2. Community Healthcare Organisation (CHO), Area 6
Abstract
Aims
Our aim was to establish which hospitals in Ireland are running oxygen clinics and to compare oxygen prescription in hospitals to a guideline standard. Long term oxygen therapy is known to be of benefit to a specific cohort of patients but is not without risk.
Methods
We sent an online questionnaire and followed up by phone to representatives in Irish hospitals in which domiciliary oxygen is prescribed. We obtained responses from 32 hospitals.
Results
Twelve hospitals (38%) had a dedicated oxygen assessment clinic while twenty (62%) did not. Centres without oxygen clinics generally prescribed oxygen following an in-patient stay 18/23 centres (78%) and were unable to provide follow up for patients on oxygen in 6/23 centres (26%). Centres with oxygen clinics generally met criteria for initial assessment and oxygen prescription, however titration of oxygen and general follow up did not meet guideline recommendations.
Conclusion
Due to a lack of dedicated oxygen assessment and review services, many Irish patients are not optimally treated with domiciliary oxygen.
Keywords: COPD, Oxygen Prescribing
Introduction
Oxygen is a recognised adjunctive treatment for patients with chronic obstructive pulmonary disease (COPD) and other chronic diseases. Long term oxygen therapy (LTOT) offers a survival benefit and improves pulmonary haemodynamics in patients with stable COPD with a resting PaO2 of <7.3 kPa. It is the only treatment for COPD that has been shown to improve mortality to date and it’s benefit was confirmed in a number of landmark trials1, 2. It addresses specific physiologic criteria and should not be confused with palliative oxygen therapy for symptomatic relief for breathless patients. The Nocturnal Oxygen Therapy Trial showed that patients receiving oxygen for 12 hours per day had a higher mortality than patients receiving oxygen for 24 hours per day1. These benefits were not seen in patients with moderate hypoxaemia or a PaO2 7.4-8.7kPa3. Furthermore, In hypoxaemic COPD patients with PaO2 of <7.3kPa, lack of provision of LTOT is an independent risk factor for hospital admission with a COPD exacerbation4.
A number of studies have shown that allowing for a period of clinical stability prior to prescribing oxygen therapy significantly reduced the numbers of patients who required oxygen at 2 months and 1 year5. This is particularly relevant to the Irish setting given the large volume of oxygen prescriptions commenced immediately following an exacerbation. Furthermore oxygen therapy is expensive with annual costs of €8.9 million in Ireland6. Many patients do not have adequate follow up, standardised prescription or accurate titration due to under-funding of services and a lack of dedicated oxygen assessment and review clinics. At present, there is no accurate data available pertaining to how many people are using LTOT in Ireland and there are no figures available on the overall cost.
Methods
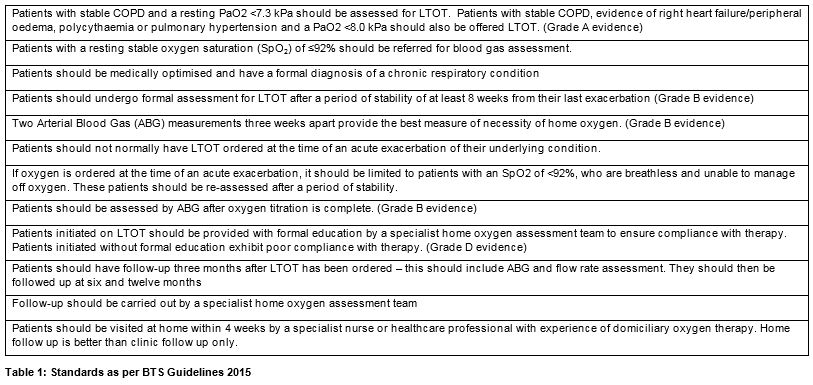
We designed this study to audit the currently provided services in Ireland and garner further insight into the number of people using LTOT and the overall cost. We postulate that there are large numbers of Irish patients who are receiving oxygen unnecessarily, still others who are not followed up appropriately and others who need oxygen and are not receiving it. We explored which hospitals in Ireland are running oxygen clinics and compared current oxygen prescription in hospitals with and without oxygen clinics to a gold standard: the British Thoracic Society Guideline for Home Oxygen use in Adults7. These guidelines have included standards for the provision of oxygen therapy which have gained international recognition. (Table 1). An online questionnaire was sent to every Irish hospital from which domiciliary oxygen is prescribed. The questionnaire was subsequently followed up by phone. Questions pertained to oxygen prescription, patient evaluation, patient follow up, titration and plans for expansion of services (table 2). The replies were compared with the established standards.

Results
We received responses from 35 hospitals in Ireland. Of the 35 hospitals, 12/35 (34%) had a dedicated oxygen assessment clinic while 23/35 (66%) (including three paediatric hospitals) did not. Centres with and without oxygen assessment and review clinics were dealt with separately.
In the 23 centres without dedicated respiratory clinics, general and respiratory physicians prescribed oxygen in 14/23 (61%) of centres. No centres without oxygen clinics had a local policy in place for staff without prescriptive authority to prescribe oxygen, and all centres had oxygen prescriptions signed off by medical staff. 18/23 centres (78%) reported primarily prescribing oxygen from in-patient wards. 11/23 centres (48%) prescribed from general, respiratory or nurse-led clinics and 4/23 centres (17%) prescribed from acute medical units.
Thirteen centres (57%) reported requiring patients to be medically stable prior to prescription of oxygen and 11/23 centres (48%) required patients to be optimised medically prior to prescription of oxygen. Eighteen centres (78%) carried out a six minute walk test (6MWT) and 21/23 (91%) carried out an ABG prior to oxygen prescription. Four centres (17%) stipulated that assessments were only done after 8 weeks of medical stability, and 8/23 (35%) stipulated that they carried out only one assessment prior to prescribing oxygen. No centre without an oxygen assessment and review clinic had any administrative support for the prescription of oxygen. Respondents from 13/23 centres (57%) reported spending over 20 minutes per patient specifically on administrative work relating to oxygen prescription.
We assessed follow up of patients who had been prescribed oxygen. Six centres (26%) reported having no formal follow up in place for patients prescribed oxygen. Thirteen centres (57%) reported following up oxygen therapy at the patient’s usual respiratory or general out-patient department (OPD) follow up, however almost all of these centres stipulated that follow up was ad hoc and resource-dependent. It is clear from the responses that a review of a patient’s specific oxygen therapy was not routinely carried out at these general respiratory OPD appointments. No centre without an oxygen clinic automatically provided patients prescribed oxygen from an in-patient setting with a follow up appointment.
Wall based oxygen was used to titrate for a home concentrator in 12/23 centres (52%), one centre had a clinic-based home concentrator and one centre used oxygen cylinders. 5/23 centres (22%) reported oxygen was not titrated.
With regards to titration for ambulatory oxygen, 8/23 centres (61%) used walk testing to maintain saturations >90%. No titration occurred in 9/23 (61%) centres. Seven centres (61%) could titrate patients on home equipment. Four centres (17%) were in a position to offer home visits carried out by Community Intervention teams or Outreach teams, while 19/23 centres (83%) did not offer home visit. Only 4/23 centres (17%) maintained a register of patients on oxygen.
Twelve of thirty-five centres who responded (34%) reported running an oxygen assessment and review clinic. Three centres (25%) were run by respiratory physiotherapists, 4/12 (33%) by respiratory nurse specialists and 5/12 (42%) by a team of respiratory nurses and physiotherapists. Seven centres (58%) had staff excluding doctors who had prescriptive authority. Five centres (42%) did not, and prescriptions were generally signed off by medical staff. Four centres (33%) reported having a local policy in place for staff without prescriptive authority to prescribe oxygen. Seven centres with oxygen assessment and review clinics (58%) maintained a register of patients on oxygen while 5/12 (42%) had no register. Six centres (50%) provided home visits, mainly by the COPD outreach teams. The waiting list to be seen in an oxygen clinic was variable. One centre had a 6 month waiting list, one was 2 months, and 7 centres had a 4-8 week waiting list. Referrals primarily came from respiratory out-patients (all centres), from in-patient teams in 9/12 centre (75%) and other healthcare providers in 3/12 centres (25%). Only 1 centre accepted direct GP referrals. 10/12 centres (83%) accepted non-respiratory patients (e.g. cardiac, palliative care) to the oxygen clinic.
With regards to titration of oxygen: 10/12 centres (83%) used walk testing to maintain saturations >90%. Only one centre tested as per guidelines: with a washout period between testing and establishing the patient on oxygen prior to starting test. 5/12 centres (42%) used wall based oxygen to titrate for home oxygen, while 4/12 centres (33%) used oxygen cylinders to titrate. Only one centre had a clinic-based home concentrator while one centre did the titration on the patient’s home concentrator.
In the case of in-patients prescribed oxygen on discharge following an in-patient stay, 8/12 centres (67%) provided an automatic follow-up appointment in the oxygen clinic while 4/12 centres (33%) did not. 9/12 centres (75%) would only carry out assessments after 8 weeks of medical stability while 3/12 centres (25%) carried out assessments at any time. Six centres (50%) carried out only one oxygen assessment before prescribing while 5/12 centres (42%) carried out two assessments, and 3/12 centres (25%) specified that they carried out two assessments three weeks apart prior to the prescription of home oxygen. All centres carried out a 6MWT and an ABG when assessing for oxygen. Six centres (50%) did not have administrative support while all centres felt there was a need for administrative support. 7/12 centres (58%) spent over 30 minutes per patient on administrative work.
Discussion
This report suggests that oxygen prescribing in Ireland requires increased resources and implementation of local guidelines in order to facilitate standardisation of treatment. As per guidelines, all patients with stable COPD and a resting PaO2 <7.3 kPa and/or SpO2 ≤92% should be assessed for LTOT7. Currently, due to a lack of dedicated oxygen assessment and review services, many Irish patients are not optimally treated with adjunctive domiciliary oxygen. Of 36 respondents to this survey, 23 hospitals (72%) did not have an oxygen assessment and review clinic. Respondents without an oxygen clinic cannot systematically offer adjunctive oxygen therapy to all eligible patients.
Most patients in centres without oxygen clinics are prescribed oxygen following an admission with an exacerbation of their chronic lung disease. This is not in keeping with best-practice guidelines, as these patients are not medically stable – guidelines recommend 8 weeks of medical stability prior to evaluation7.
This report also finds that in these centres no patients are automatically provided with an appointment to follow up their home oxygen therapy following prescription on the ward. This finding suggests that there may be a large number of patients currently on oxygen in the community who may not require it, with significant cost implications to healthcare provision in Ireland. Observational studies have shown that among patients supplied with LTOT from hospital discharge or during a period of clinical instability, 30-58% of them no longer required oxygen 1-3 months later8.
Centres with oxygen clinics generally met criteria for initial assessment and oxygen prescription, however titration of oxygen and general follow up did not meet the gold standard objectives. Most centres running oxygen clinics required their patients to be medically stable with optimised medical treatment prior to prescription of oxygen. In terms of long term oxygen prescription, no centres met full BTS criteria of 2 assessments, 3 weeks apart carried out after an 8 week period of medical stability.
The lack of formal follow up for many patients prescribed domiciliary oxygen is clear from this report. Not enough centres are offering home visits for patients prescribed oxygen therapy. Very few patients are visited within four weeks as per the standard, and thorough education regarding oxygen therapy cannot be provided in the general outpatient setting.
To address the current shortcomings in oxygen prescription and review services in Ireland, we would make a number of recommendations. It is our belief that the development of regional centres providing oxygen assessment and review (OAR) clinics which have capacity to provide home visits and link with community respiratory teams should be funded and prioritised. The paediatric population requires dedicated OAR and ventilation clinics with capacity to provide home visits and link with community respiratory teams. Furthermore, we recommend that each OAR clinic be staffed with a Respiratory/Oxygen Clinical Nurse Specialist and a Physiotherapist. National Key Performance Indicators should be established to ensure OAR clinics are meeting the standards required, and a nationally held electronic database of patients attending OAR clinics should be established. OAR clinic should be provided with an administrator responsible for general administration, maintenance of oxygen register and data management. OAR clinic staff should ensure the roll out of new respiratory therapy contracts is in line with HSE requirements. From this study, it is clear that there is a need for improved access to, monitoring and regulation of oxygen delivery in Ireland, and we feel that the above recommendations provide an effective framework to achieve this.
Conflicts of Interest Statement
All authors have no conflicts of interest to declare.
Corresponding Author
Dr. Cliona O’Donnell
St. Vincent’s University Hospital,
Dublin
Email: [email protected]
ORCID ID: 0000-0001-8882-8889
References
1. Nocturnal Oxygen Therapy Trial G. Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: A clinical trial. Annals of Internal Medicine. 1980;93(3):391-8.
2. J Leggett R, Cooke N, Clancy L, G Leitch A, Kirby B, C Flenley D. Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Report of the Medical Research Council Working Party. Lancet 1981 1 681 686 61109121976. 414-8 p.
3. Górecka D, Gorzelak K, Sliwiński P, Tobiasz M, Zieliński J. Effect of long-term oxygen therapy on survival in patients with chronic obstructive pulmonary disease with moderate hypoxaemia. Thorax. 1997;52(8):674.
4. Ringbaek TJ, Viskum K, Lange P. Does long-term oxygen therapy reduce hospitalisation in hypoxaemic chronic obstructive pulmonary disease? European Respiratory Journal. 2002;20(1):38.
5. Timms RM, Kvale PA, Anthonisen NR, Boylen CT, Cugell DW, Petty TL, Williams GW. Selection of patients with chronic obstructive pulmonary disease for long-term oxygen therapy. JAMA. 1981;245(24):2514-5.
6. National Reform Programme.
7. Hardinge M, Annandale J, Bourne S, Cooper B, Evans A, Freeman D, Green A, Hippolyte S, Knowles V, MacNee W, McDonnell L, Pye K, Suntharalingam J, Vora V, Wilkinson T. British Thoracic Society guidelines for home oxygen use in adults: accredited by NICE. Thorax. 2015;70(Suppl 1):i1.
8. Levi-Valensi P, Weitzenblum E, Pedinielli J-L, Racineux J-L, Duwoos H. Three-Month Follow-Up of Arterial Blood Gas Determinations in Candidates for Long-Term Oxygen Therapy. American Review of Respiratory Disease. 1986;133(4):547-51.
P933
