Patient Texting in General Practice: Who, Why, Why Not? A National Survey of Text Messaging in Irish General Practice.
Quinlan D1, Dahm M2, Lyons A3, Collins C4
1Woodview Family Doctors, Kearney's Cross, Sallybrook, Riverstown, Glanmire, Co. Cork
2Clonakilty Family Health Clinic, Faxbridge Shopping Complex, Clonakilty, Co Cork
3General Practitioner, HSE South
4Director of Research & Innovation, Irish College of General Practitioners, 4-5 Lincoln Place, Dublin 2
Abstract
Introduction
The benefits of text messaging patients are well documented. The General Medical Council recently published guidance endorsing text messaging. The use of text messaging by GPs in Ireland is currently unknown. The survey aims to address this knowledge deficit and ascertain the extent, benefits, risks, barriers and clinical role of text messaging in Irish general practice.
Methods
An online survey was emailed to 1,375 members of the Irish College of General Practitioners (ICGP).
Results
A total of 536 GPs completed the questionnaire; a response rate of 40%. Overall, 66% (n=353) of respondents text patients and 27% have a written policy for texting patients. Texting is used primarily to send test results (71%), to advise the patient to phone the practice (52%) and as appointment reminders (43%).
Discussion
GPs text messaging patients is widespread. Complex issues to resolve include consent, confidentiality, children/young adults and the clinical content of text messages. Guidance is required to enable GPs and patients harness the benefits of text messaging, while minimising potential risks.
Introduction
The potential benefits of text messaging to help improve the care of patients are beginning to emerge, for example in improving psychiatric outpatient attendances1 and improving smoking cessation2. A recent Cochrane review concluded that there are “significant information gaps regarding effects, risks and limitations and user satisfaction” with text messaging as a tool for enhancing preventative health care3. The UK General Medical Council (GMC) recently endorsed text messaging patients as both convenient and effective, provided reasonable steps to protect confidentiality are undertaken4. The Irish Medical Council is silent on text messaging. The office of the Data Protection Commissioner recommends that text messaging be limited to non-clinical matters. Both medical indemnity organisations for GPs in Ireland advise caution in text messaging patients, specifically advising that personal clinical information should not be sent by text5. The use of text messaging by GPs in Ireland is currently unknown. The aim of this survey was to ascertain the extent, benefits, risks, barriers and clinical role of text messages in Irish general practice.
Methods
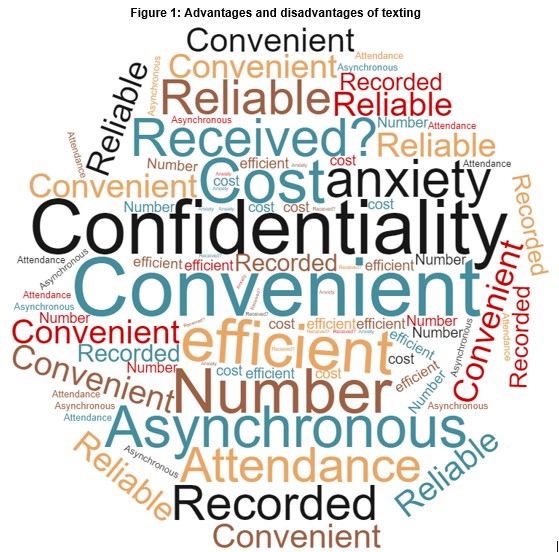
An online survey using Survey Monkey was emailed to 1,375 members of the College of General Practitioners (ICGP). Two reminders were sent, one and two weeks later. The authors developed the questionnaire to ascertain extent, perceived risks, benefits, barriers and clinical utility of text messaging from the GP perspective. Survey data was subject to simple descriptive statistical analysis using SPSS (version 25). Chi-square test was used to test relationships with a p-value of 0.05 considered significant. A thematic analysis was undertaken in terms of the open-ended questions relating to the advantages and disadvantages of the use of texting and a word cloud utilised to summarise this data.
Results
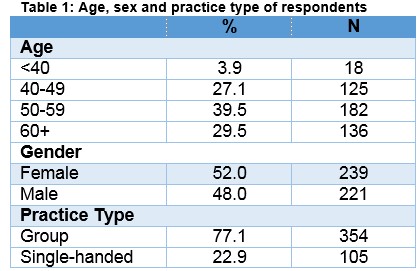
A total of 536 GPs completed the questionnaire; representing a 40% response rate. The profile of respondents is similar to ICGP membership (Table 1).
Overall, 65.9% (n=353) of respondents text patients. Of these, 6.8% (n=22) initiated texting before 2010 and since then there appears to have been a steady increase each year. However, approximately one quarter (26.7%; n=86) have a written text policy for texting patients. A total of 16.1% (n=52) reported a previous negative experience texting patients. Whether GPs text or not was not related to age group but was related to gender with females significantly more likely to use texting (74.9% compared to 62.9% of males; p<0.01); which exists whether the GP works full-time or part-time. Overall, 61.2% (n=197) of GPs who use texts always document patient consent; 28.9% (n=93) sometimes document consent and 9.9% (n=32) never document patient consent. When texting medically sensitive information 55.6% (n =179) always obtain specific consent, 20.8% (n=67) sometimes and 23.6% (n=76) never obtain specific consent to text medically sensitive information.
Respondents were provided with a list of options and asked to indicate why they text patients. Overall, 77.3% (n=249) reported texting the patient test results, 51.9% (n=167) to advise the patient to phone the practice, 46.6% (n= 150) as appointment reminders, 16.5% (n=53) for sending other medical information, while 16.8% (n= 54) use texting to communicate ‘other’ information. Examples of such include answering a patient query (n=11), communicating with patients who have hearing difficulties (n=3), or sending non- medical information (such as to advise the patient that an item is ready for collection (n=6), that their medial card has expired (n=4) and to send links or phone numbers for services (n=2)). Just 22% (n=71) of GPs currently send text messages to patients aged 16 or 17 years while only 3.7% (n=12) text patients under the age of 16 years.
GPs who send text messages report the main advantages as those related to efficiency and convenience, with time management the overwhelming advantage mentioned specifically by 34.2% (n=109). The next most often cited advantages were cost and saved doctor having an additional phone consultation both mentioned by 8.8% (n=28) of respondents. These GPs report the main disadvantage as potential confidentiality breach, which was mentioned directly by 21% (n=66) and indirectly by 27.1% (n=85) who referred to the fear of sending the message to the wrong person/number with an additional 18.2% (n=57) referring to the lack of certainly around receipt (Figure 1).
Similarly, GPs who currently do not text patients, identify time management as the perceived principal benefit. The risk of breaching confidentiality emerged as the greatest barrier to text messaging patients.
The primary reason for not sending texts is potential breach of confidentiality, as reported by 21.2% (n=31) of respondents who do not use text messaging. The main confidentiality issues surround texting the wrong person (9.6%, n=14). Others mention logistical reasons, such as added time (7.5%, n=11) and workload (5.5%, n=8), and the added cost (2.7%, n=4). Unfamiliarity with web texting was also cited (7.5%, n=11). Respondents also identified data protection concerns (7.5%, n=11), with a minority (2.4%, n=4) mentioning medical indemnity organisations advising against use of text. Almost half (48.6%; n=71) of those who do not currently text patients would commence texting if endorsed by the ICGP, Medical Council and indemnity organisations.
Discussion
This study met the objective to ascertain the extent, benefits, risks, barriers and clinical role of text messages in Irish general practice. Two thirds of Irish GPs currently text their adult patients. The overwhelming benefit is enhanced time management. The potential to breach patient confidentiality emerges as the principal risk of text messaging. Almost half of GPs who do not currently text patients would initiate text messaging with appropriate support and clinical governance. Text messages convey both clinical and administrative information to patients.
The uptake of texting by GPs has been increasing since 2010, especially since 2014 onwards, in the absence of Irish Medical Council guidance, well in advance of recent GMC guidance, and despite concerns expressed by the MPS, Medisec and the Office of Data Protection Commissioner. It is of concern that written consent to text patients is not always obtained by approximately one third of GPs. Of equal concern is that just 56% of GPs always document consent to text medically sensitive information. GPs are clearly cautious about sending text messages to young adults (16y, 17y). There are specific challenges sending texts to young adults (changing mobiles, shared phones). It is important to recognise this group of digital natives, are legally capable of consenting to such communication. GPs should not discriminate against them, while at the same time recognising the risks and ensuring appropriate controls are in place. It is notable that 66% of GPs text patients and almost half of “non-texters” would initiate text messaging patients if endorsed by the ICGP, Medical Council and indemnity organisations. Such a change would evolve text messaging patients to an everyday clinical activity.
GPs describe confidentiality as the greatest concern with text messaging and the greatest barrier to initiating text messaging. This accords with the Irish Medical Council guidance “Confidentiality is central to the trust…and a core element of the doctor/patient relationship…You should protect your patients’ privacy (and) guard against accidental disclosures”6. The GMC acknowledge the balancing required “you should communicate with patients in a format that suits them. For example…text messaging…Most communication methods pose some risk of interception – for example, (overheard) messages left on answering machines”4. The content of a text message to patients must be carefully considered, bearing in mind that it may never reach the patient, or that others may read the text. Clearly, text messaging alone is inappropriate for urgent or important messages.
GPs clearly described time management as the overwhelming benefit to text messaging patients. The long hours worked by GPs are well documented, with GP recruitment and retention in crisis7. International research identifies “a seemingly endless demand for consultations, coupled with more complex patient care, escalating administrative tasks, pressures to meet quality performance targets, and rising documentation requirements”7. Ireland has too few GPs and is below the OECD average in this regard. Ireland has just 64 GPs per 100,000 population, versus 80 GPs per 100,000 in Scotland, representing 20% fewer GPs7. Consequently, GP time management is fundamental to enable sick patients obtain same-day access to their GP - text messaging may liberate GP “time to care”. This study is the first national survey of Irish GPs opinions about texting and may be subject to response bias, whereby GPs who send text messages were more likely to respond to this survey. However, the response rate of 40% of all ICGP members represents a very substantial cohort of opinion. A survey such as this cannot capture the nuances and complexities of communication between doctors and patients and as such does not offer a full picture of the nature of text messaging which occurs.
A limitation of these findings is that they represent self-reported use, however, a clear strength is the relatively high response rate, which is in excess of the typical response rate to such surveys within general practice8-10. The findings demonstrate that GPs text messaging patients is currently widespread, yet remains an area lacking research. Complex issues to resolve include consent, confidentiality, children/young adults and the clinical content of text messages. The key stakeholders - ICGP, indemnity organisations, the Irish Medical Council, data protection officials and patient representatives – should urgently develop guidance to enable GPs and patients harness the benefits of text messaging, while minimising potential risks. The final decision to receive text messages must rest with each patient, expressing or withholding informed consent, following a discussion of the risks, benefits and limitations of text messaging.
Conflict of Interest
The authors nor the authors’ institution has financial or personal relationships with other persons or organizations that inappropriately influence (bias) their actions.
Corresponding author:
Claire Collins, Director of Research & Innovation, Irish College of General Practitioners, 4-5 Lincoln Place, Dublin 2. Phone: 01 676 3705;
Email: [email protected]
References
1. Sims H, Sanghara H, Hayes D, Wandiembe S, Finch M, Jakobsen H, Tsakanikos E, Okocha CI, Kravariti E. Text Message Reminders of Appointments: A Pilot Intervention at Four Community Mental Health Clinics in London. Psychiatr Serv. 2012 Feb 1;63(2):161–8.
2. Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth Chronic Disease Management on Treatment Adherence and Patient Outcomes: A Systematic Review. J Med Internet Res [Internet]. 2015 Feb 24;17(2). Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4376208/
3. Vodopivec-Jamsek V, de Jongh T, Gurol-Urganci I, Atun R, Car J. Mobile phone messaging for preventive health care. Cochrane Database Syst Rev. 2012 Dec 12;12:CD007457.
4. Confidentiality: good practice in handling patient information GMC April 2017 [Internet]. [cited 2017 Aug 3]. Available from: http://www.gmc-uk.org/static/documents/content/Confidentiality_good_practice_in_handling_patient_information_-_English_0417.pdf
5. Texting, faxing and emailing patients [Internet]. [cited 2017 Aug 3]. Available from: http://www.medisec.ie/a-z/texting-faxing-and-emailing-patients
6. Guide to Professional Conduct and Ethics for Registered Medical Practitioners 8th Edition 2016 [Internet]. [cited 2017 Aug 3]. Available from: http://www.medicalcouncil.ie/News-and-Publications/Reports/Guide-to-Professional-Conduct-and-Ethics-8th-Edition-2016-.pdf
7. ‘Manpower and General Practice’ Joint Oireachtas Committee on Health, ICGP Opening Statement [Internet]. [cited 2017 Aug 3]. Available from: https://www.icgp.ie/go/library/catalogue/item/F4DAB7D0-F280-F484-CA1C3518B6836F50?highlight=manpower
8. Crowley D, Collins C, Delargy I, Laird E, Van Hout MC. Irish General Practitioner attitudes toward decriminalisation and medical use of cannabis: Results from a National Survey. Harm Reduction Journal 2017: 14(4). DOI: 10.1186/s12954-016-0129-7.
9. Streit S, Verschoor M, Rodondi N, Bonfim D, Burman RA, Collins C, Gerasimovska KB, Gintere S, Bravo RG, Hoffmann K, Iftode C, Johansen KL, Kerse N, Koskela TH, Peštić SK, Kurpas D, Mallen CD, Maisoneuve H, Merlo C, Mueller Y, Muth C, Šter MP, Petrazzuoli F, Rosemann T, Sattler M, Švadlenková Z, Tatsioni A, Thulesius H, Tkachenko V, Torzsa P, Tsopra R, Canan T, Viegas RPA, Vinker S, de Waal MWM, Zeller A, Gussekloo J, Poortvliet RKE. Variation in GP decisions on antihypertensive treatment in oldest-old and frail individuals across 29 countries. BMC Geriatrics 2017: 17(93) DOI 10.1186/s12877-017-0486-4
10. McAvoy BR, Kaner EFS. General practice postal surveys: a questionnaire too far? BMJ. 1996: 313(7059): 732.
(P729)
