Patients’ Attitude towards Travelling For Breast Services versus Waiting Longer For Local Services
Abd Elwahab S., McGough P, Cooley G, McLaughlin R.
Symptomatic Breast Unit, University College Hospital Galway
Abstract
Geographical access is a cornerstone of health care provision. However, prolonged waiting for breast clinic appointments in local services results in delayed diagnosis and excessive anxiety for patients. In this study, we present a patient satisfaction survey results of an initiative to offer out-patient clinic appointments for non-urgent patients referred to the breast unit in Letterkenny General Hospital (LGH), Ireland, and exceeded the recommended waiting period of 12 weeks. These patients were offered appointment in University Hospital Galway (UCHG), which is an average travel time of about 3.5-4.5 hours away from LGH. 163 patients out of 336 (48.5%) patients actively waiting more than 12 weeks for appointments in LGH accepted alternative appointments in UCHG. Despite the long travel distance for these patients, 100% of them reported high satisfaction and 97.3% said they would accept further UCHG appointments if a similar situation of prolonged waiting in LGH arises. None of these patients were diagnosed with cancer, and only one had a benign lumpectomy. This study showed that if offered alternative appointments, just under half of the patients would accept. The initiative provides a feasible solution for long waiters, and the survey shows that patients’ satisfaction remains high despite long travel.
Introduction
Geographical access to clinical breast care facilities is a significant factor in healthcare planning, but its impact on clinical outcome has been a debatable issue1. Some studies suggested that patients who lived farther away from clinical services and rural residents were disadvantaged regarding breast care and screening, and usually suffer delayed diagnosis as a result1,2. Other studies found that travel distance and geographical access did not affect cancer diagnosis and was not a significant factor in terms of timing and stage of disease. Henry et al suggested that other factors like public transportation, clinic capacity, and travel costs might have more impact than travel distance3,4.
North-west Ireland is geographically unique. County Donegal, and its regional hospital, Letterkenny General Hospital (LGH), are part of Saolta Hospital Group that serves that region of Ireland. The geography and healthcare access of Donegal has been a concern in planning of healthcare service. Following the national report on centralization of hospital services (The Hanley Report), R Kalogirou et al. predicted that access to hospital service in the western and central regions of Ireland would be negatively impacted by the formation of hospital groups. They used Geographical Information Systems (GIS) in their analysis and prediction which mainly relies on environmental and geographical data5. Due to this unique geography, LGH has a symptomatic breast unit that is a sub-centre of and directly linked to the central breast service in University College Hospital Galway (UCHG)6. Both units closely follow the NCCP and HSE guidelines that regulate breast clinic appointments and referral. General practioners (GP) referrals are triaged centrally in UCHG and patients are offered appointments in different centers based on patient’s address and geographical allocation; with maximum waiting period of 12 weeks for routine appointment as per National Cancer Control Program(NCCP) guidelines7.
Waiting times for symptomatic breast appointments have been an issue of national public concern and a subject of media attention8. Through the NCCP key performance indicators, it was flagged that LGH had exceeded the standard limit of 12 weeks for numerous reasons. These patients are all in the routine category of triage (low risk of cancer diagnosis), and as per the NCCP guidelines should be seen within 12 weeks of referral.
The solution applied was to offer these patients appointments in UCHG instead, which is the nearest breast center. The distance between LGH and UCHG is about 251 km, with a travel time ranging between 3.5 to 4.5 hours depending on means of transportation, road and traffic conditions. Geography and travel distance were thought to be a significant challenge, however, there is still a debate and lack of conclusive evidence on its specific impact on breast care service3,9,10. Also, to the best of our knowledge, there is still no published literature regarding patients’ preferences in terms of traveling relatively long distance versus prolonged waiting periods for local breast care access. In this survey, we aimed to study the impact of relatively long travel to breast care facilities on patient compliance and satisfaction in Irish hospital group setting.
Methods
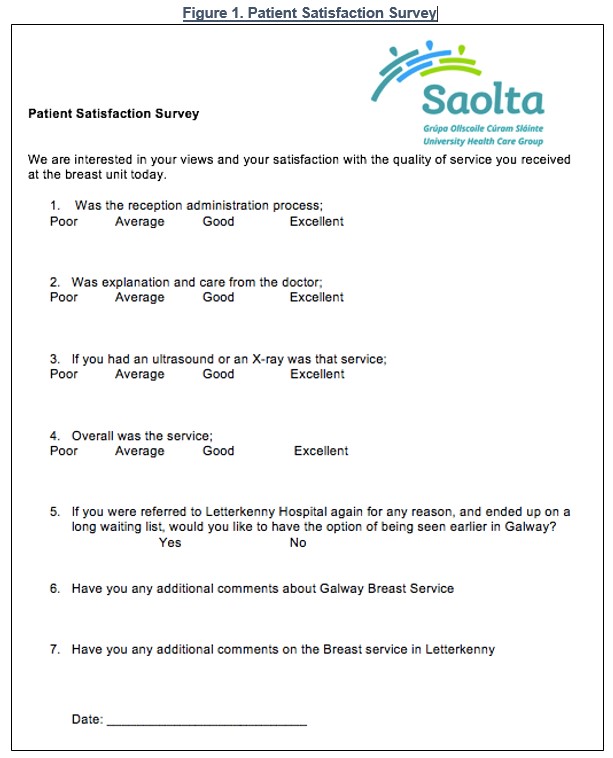
The study aimed at determining compliance rate of clinic appointments for those from Donegal and would normally be seen in LGH but were offered appointments in UCHG because their waiting time exceed the guidelines limit of 12 weeks. These appointments were offered in pre-scheduled clinics so their financial impact on the UCHG unit was minimal. The rate of non-attendance and declining a UCHG clinic appointment was calculated as a measure of compliance, and a patient satisfaction survey and feedback was done to assess the impact of travel. A patient satisfaction questionnaire was given to the patient on arrival to clinic at the check-in desk to fill. The questionnaire was designed to be simple, direct, and capture the overall satisfaction, as well as satisfaction with specific various stages of triple assessment clinic including: reception/ administrative area, clinical interview, and radiology section. The answers were designed to use the Likert four-point scale. There was a section to allow free-hand feedback and comments about both LGH and UCHG (please see questionnaire in figure 1 below). Analysis was done using STATA statistical software version 12.
Results
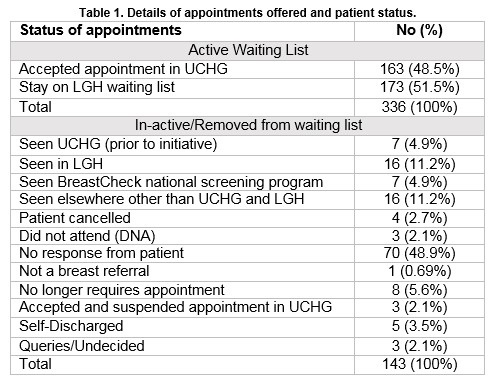
This initiative started on February 2016 after discussion and approval by breast surgeons in UCHG and LGH. At the start of the initiative, 479 patients were found to be waiting for appointments for more than 12 weeks in LGH, only 336 (70.1%) were actively awaiting appointments (the rest were either missed their appointment, offered an appointment and wanted to re-schedule or did not attend an offered appointment). All those on the active waiting list were offered alternative appointments in UCHG, priority was given to those waiting longest. One hundred and sixty-three (48.5%) accepted these alternative appointments.
Of those 163 patients, only three patients (1.8%) did not attend (DNA) the clinical appointment after accepting it; appointment compliance rate was 98.2%. Please see table 1 below for details.
All patients were females, with a mean age 45.2 (SD±15.9) years (median 43 years; range 12-91 years). The survey questionnaire was offered to these patients on arrival to the clinic, 85 of them (52.1%) participated. Please see table two below for details.
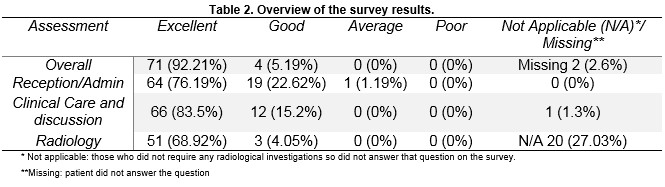
When asked if she would accept another UCHG appointment should a similar situation of long waiting for LGH appointment arises, 97.37% of the patients (74) responded that they would accept a UCHG appointment, and only 2 patients (2.63%) said that they would not.
On free hand comments section, 26 patients commented that UCHG breast unit was professional, friendly and well organized. Three patients thought that LGH requires more staff, 11 commented that the waiting period is unacceptable. Although not part of the survey, only one patient in this cohort had surgery for a benign radial scar.
Discussion
Our results indicate that almost half of the long waiters would accept (48.5%) alternative breast clinic appointments that involve long travel and that it did not affect patient satisfaction. These patients generally preferred to get a timely appointment in a farther center rather wait longer for one in a local facility. This study showed that patients do not object travelling to get the necessary care. The compliance rate was relatively high. This might indicate high levels of anxiety to get access and address breast complains.
These long waiting patients are at risk of being diagnosed with more advanced stages of breast cancer due to their dis-advantage of geographical access to service2. Fortunately, as mentioned above, none of the patients in our cohort was diagnosed with breast cancer, and only one patient required a lumpectomy operation for a benign radial scar. The patient decided to have the operation in UCHG despite being offered the option of surgery appointment in LGH. Having no cancer patients in this cohort indicates that triage system was efficient and reliable. This was key to the success of this initiative which depends on identification of non-urgent patients and those that are unlikely to require surgical intervention which will increase burden on patients and the service. The feedback and comments reflected that patients maintained a high regard for their local LGH center as well as insight to issues such as understaffing. At the same time, they showed gratitude and high satisfaction with the efforts to try solving long waiting times even if it involved long travel.
The disadvantages of our plan, other than patient inconvenience and troublesomeness, were increasing workload on other non-local centers. Judicious use of available outpatient time was crucial in the planning phase of this initiative as well as communication with all the clinical, radiological, nursing and administrative teams in the UCHG breast clinic. One of this study limitations is that it only surveyed patients who attended UCHG, as opposed to all the patients including those who elected not to attend. Efforts were made to try to reduce this bias by offering these questionnaires to those who declined these alternative appointments. This failed due to logistical reasons and lack of personnel to conduct the survey in Letterkenny. Additionally, these patients’ details were not made available to our center once they rejected the alternative appointments. However, despite this limitation, we present a possible solution to waiting list problems in areas where geographical access is an issue. Our survey shows that long waiters were likely to accept and were highly satisfied when offered appointments in other centers that involved longer travelling. This suggests that distributing breast clinic appointments to other centers within the geographical hospital group might be a reasonable solution to prolonged breast clinic waiting periods and that it does not negatively impact on patient satisfaction.
Conflict of interest:
None
Correspondence:
Sami Abd Elwahab, Symptomatic Breast Unit, University College Hospital Galway
Email: [email protected]
Mobile: 0871441351
References
1. Celaya MO, Berke EM, Onega TL, Gui J, Riddle BL, Cheralla SS, Rees JR. Breast cancer stage at diagnosis and geographic access to mammography screening (New Hampshire, 1998-2004). Rural and remote health. 2010;10:1361.
2.Nguyen-Pham S, Leung J, McLaughlin D. Disparities in breast cancer stage at diagnosis in urban and rural adult women: a systematic review and meta-analysis. Annals of epidemiology. 2014;24:228-235.
3.Alford-Teaster J, Lange JM, Hubbard RA, Lee CI, Haas JS, Shi X, Carlos HA, Henderson L, Hill D, Tosteson AN, Onega T. Is the closest facility the one actually used? An assessment of travel time estimation based on mammography facilities. International journal of health geographics. 2016;15:8.
4.Henry KA, Boscoe FP, Johnson CJ, Goldberg DW, Sherman R, Cockburn M. Breast cancer stage at diagnosis: is travel time important? Journal of community health. 2011;36:933-942.
5.Kalogirou SF, Ronan. Health, place and Hanly: Modelling accessibility to hospitals in Ireland. Irish Geography 2006;39:52-68.
6.Health Service Executive (HSE). Letterkenny General Hospital. URL: http://www.hse.ie/go/LGH/. Accessed on March 2016.
7.National Cancer Controll Program (NCCP). GP Breast Referral Guidelines 2009.. URL: https://www.hse.ie/eng/services/list/5/cancer/profinfo/resources/gpreferrals/gp-guidelines-and-referral-forms.html. Accessed March 2016
8.Donnellan, E. Waiting times for breast clinics breach guidelines. The Irish Times. May 26th, 2009.
9.Lamont EB, Hayreh D, Pickett KE, Dignam JJ, List MA, Stenson KM, Haraf DJ, Brockstein BE, Sellergren SA, Vokes, EE. Is patient travel distance associated with survival on phase II clinical trials in oncology? Journal of the National Cancer Institute. 2003;95:1370-1375.
10.Onega T, Hubbard R, Hill D, Lee CI, Haas JS, Carlos HS, Alford-Teaster J, Bogart A, DeMartini WB, Kerlikowske K, Virnig BA, Buist DS, Henderson L, Tosteson AN. Geographic access to breast imaging for US women. Journal of the American College of Radiology : JACR. 2014;11:874-882.
(P754)
