Patterns of Mortality in Modern Stroke Care
M D'Alton, T Coughlan, N Cogan, S Greene, DJH McCabe, A McCarthy, S Murphy, R Walsh, D O’Neill, S Kennelly, D Ryan, R Collins.
Age-Related Health Care/Stroke-Service, Tallaght Hospital.
Abstract
Background
Stroke is a leading cause of death. We looked at the causes (direct and indirect) of in-hospital mortality in a modern stroke unit over a two-year period.
Methods
We reviewed medical charts of stroke deaths in hospital from 2014-2015 inclusive. Data on stroke type, aetiology, age, length of stay, comorbidities, and documented cause of death were recorded. All patients were included.
Results
518 patients were admitted acutely to the stroke service. Overall death rate was 7.5% (n=39). Of fatal strokes 29 (74%) were ischaemic. Average age 78.6 years. Mean survival was 26.4 days (range 1-154). 19 (49%) patients had atrial fibrillation. Forty-nine percent of deaths were due to pneumonia, and 33% were due to raised intracranial pressure.
Discussion
Mortality rate in our stroke service has decreased from 15% in 1997, and now appears dichotomised into early Secondary Stroke Related Cerebral Events (SSRCEs) and later infections.
Introduction
Stroke is the third leading cause of death in Ireland1. In recent years there have been many developments in the management of stroke, including widespread adoption of the acute stroke unit model of care, thrombolysis, and intra-arterial thrombectomy for acute ischaemic stroke. Increased use of new oral anti-coagulants for stroke prevention, which may also ameliorate effects of an acute ischaemic event, improved access to neuroimaging, and an improvement in the quality and availability of non-acute stroke rehabilitation and secondary prevention follow up, have all improved our processes of care. With these modern advances in treatment, the incidence and causation of death after stroke may be changing. We examined the causes of in-hospital death among patients admitted to an acute stroke service over a two-year period in order to identify targets for improved outcome.
Methods
We operate a nine-bedded dedicated stroke unit in a tertiary 614-bed hospital, with a specialized multidisciplinary team and 24-hour access to thrombolysis and a thrombectomy care pathway. All acute stroke patients are admitted per clinical protocol to the acute stroke service. We maintain a database of all stroke patient admissions as part of the national stroke registry and we carried out a retrospective review of the medical charts of all patients who died in hospital following acute stroke from 2014 to 2015 inclusive. All patients were included. The cause of death was recorded as that documented on the statutory death certification form. Data were collected on stroke type, aetiology, severity of symptoms, age, major comorbidities and length of stay. Results were compared with data from the total stroke population in our service. Statistical analysis was carried out using GraphPad Prism 7©2. Demographic comparisons of deaths with the total population were made using unpaired t-tests for continuous outcomes (age and length of stay) and Fisher’s test to compare rates of atrial fibrillation and stroke type.
Results
The total number of acute stroke patients admitted to the stroke service was 261 in 2014 and 257 in 2015. 83% were cared for in the acute stroke unit, including 72% (n=18) of those who died. The death rate in the stroke service over a two-year period was 7.5% (n=39). Fifty-two patients had an admission diagnosis of stroke according to Hospital Inpatient Enquiry (HIPE) coding, but were not admitted under the dedicated stroke service, including seven patients who died (13.5%). Overall stroke mortality in the hospital in 2014-2015 was 8%. Specific demographic and clinical data were not recorded on patients outside the stroke service.
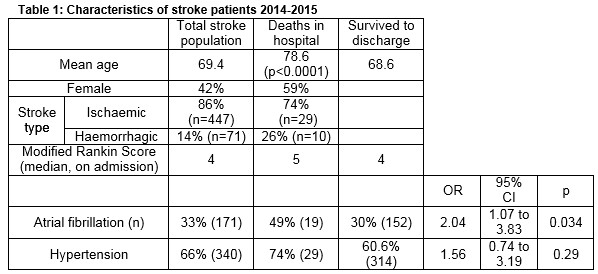
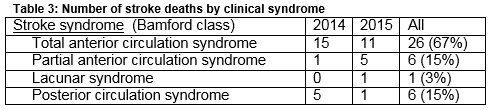
The respective death rates for ischaemic and haemorrhagic stroke were 6.5% and 14% (p=0.048). Cause of death is represented in Table 2. Of fatal strokes 29 (74%) were ischaemic. Fifty-nine percent of patients were female. The average age was 78.6 years, compared with 69.4 years in the total stroke population (p<0.0001). Table 3 gives a breakdown of deaths by stroke syndrome, showing that 26 patients (67%) had a total anterior circulation syndrome on admission. Nineteen patients (49%) had atrial fibrillation, compared with 30% of survivors (OR 2.07, p=0.03) and 33% of total stroke admissions. The death rate in patients with atrial fibrillation was 11%, compared to 5.7% in those without confirmed AF. Among stroke deaths 7 patients had active cancer and 8 had co-existing dementia.
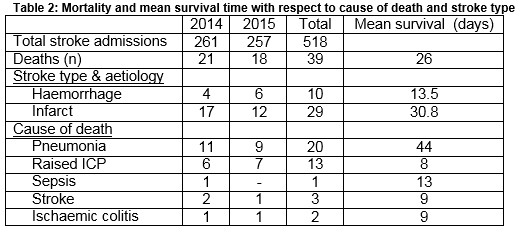
Mean survival time of those who died was 26.4 days overall (range 1-154); 31 days in ischaemic and 13.5 days in haemorrhagic stroke. Mean survival time was much shorter in those where “raised ICP” or where “primary stroke” was identified as the primary cause of death compared with pneumonia (7 vs 44 days, p=0.0002). Raised ICP was a more common cause of death in haemorrhagic stroke (70%) than ischaemic (31%). There was no significant difference in survival time with respect to stroke syndrome (by Bamford classification) among the deaths. The Modified Rankin Score (mRS) on admission was documented in 477 of our stroke patients (92%), including 37 of those who died. The median score in the group who died was 5, compared with a median mRS of 4 in survivors and in the total stroke population admitted within the same period.
Discussion
Stroke mortality has decreased to 7.5% from 15% in 1997-98, when the first audit of our stroke service was carried out3, prior to the existence of a geographical stroke unit and complete dedicated multi-disciplinary team with a 24/7 thrombolysis and thrombectomy acute care pathway. This downward trend is similarly reflected in national data from the UK, which reported mortality rates of between 21% and 33% in 1998, versus 15.3% in 20134,5. Mortality data from our unit compares favourably with both this and overall figures in Ireland, which reported death rates of 9.7% and 24.6% from ischaemic and haemorrhagic stroke respectively in 20136. Hospital In-Patient Enquiry (HIPE) data recognised an additional 52 patients (10% of total stroke population examined) with an admission code for stroke not admitted under our service. Detailed data were not captured on patients not looked after by the stroke service, however mortality was higher among this small cohort (13% vs 7.5%). This is likely to be due to a combination of discrepancy in coding, as only acute stroke patients are taken over by the stroke service, patient transfers to neurosurgical centre prior to referral to stroke team, patients with severe stroke who died at presentation or in-hospital strokes with other significant illnesses such as cancer who stayed with the initial treating teams.
In our cohort, patients who died were nine years older than the general stroke population (p<0.0001) and more likely to have atrial fibrillation (OR 2.07, P=0.033). The death rate in primary haemorrhage was higher than in ischaemic stroke (OR 2.36, P=0.048). Females were over-represented. These trends are in keeping with recent national mortality data7.
The difference in Modified Rankin Score indicates that patients who died had a greater burden of disability on admission than the total population. However, the admission MRS was not documented in all patients and there is scope to examine this in greater detail as a predictor of in-hospital mortality. Seventy-two percent of patients who died were admitted to the stroke unit, while the remainder either required intensive care unit admission or were palliated from the outset on a general medical ward.
Mortality would now appear dichotomised into early Secondary Stroke Related Cerebral Events (SSRCEs) and later infections. Diagnosis of active cancer was relevant in 7 deaths. Dementia was considered the main contributory cause of one death due to pneumonia. The main cause of early death from stroke in our cohort is raised intracranial pressure (particularly in intracranial haemorrhage) and this highlights the need for advanced treatment options, medical and surgical, to reduce the haematoma expansion and effectively decompress critical ICP patients. Positive results have been seen in recent years with surgical intervention in ischaemic stroke, where hemicraniectomy for malignant middle cerebral artery syndrome, performed within 48 hours, resulted in a mortality benefit as well as a reduction in disability in several trials8,9. While initial trials such as DECIMAL and HAMLET excluded patients over the age of sixty, more recently DESTINY II showed that there is benefit in performing surgical decompression in older patients with middle cerebral artery infarcts10.
Results have been less promising with regard to haemorrhagic stroke, for which there remains a lack of effective intervention in the acute setting, and there is still a much higher mortality rate in this cohort compared with ischaemic stroke. The STICH trial showed that there was no difference in outcome between the two groups11. Trials of medical treatment aimed at reducing haematoma size, such as factor VIIa, have also been disappointing, demonstrating no improvement in survival or functional outcome12. A phase III trial (TICH-2) is under way exploring tranexamic acid for this purpose13. Osmotic therapy with mannitol has shown possible benefit in larger volume haematomas but further evidence is needed to support this as a strategy14,15. Neuroprotective treatments for ischaemic stroke, including therapeutic hypothermia and pharmacological therapies, have also been shown to be feasible in early trials16,17.
Later death from stroke is mainly due to infection. Bedside swallow screening, while not a highly sensitive test for dysphagia, does reduce the rate of aspiration pneumonia and should be performed in all stroke patients18. However despite 93.6% of our stroke patients undergoing swallow screen at admission, there was a high rate of death due to presumed aspiration pneumonia. This may be indicative of a need for more objective swallow screening such as videofluoroscopy, but could also be explained by other factors such as immune suppression and hospitalisation in a stroke population. The association between mortality and rate of atrial fibrillation in our study population emphasises the importance of detecting and treating this condition for primary and secondary prevention of stroke. Strokes due to atrial fibrillation occurring on anticoagulation are less severe than those occurring untreated19 and atrial fibrillation may be associated with underlying diastolic heart failure, predisposing to pulmonary congestion and infection. Atrial fibrillation is also associated with recurrent stroke events and other critical ischaemic events such as Ischaemic colitis. Optimal timing of anticoagulation post stroke in patients with atrial fibrillation needs more evidence, however a number of registries on this issue are on-going and the European Stroke Organisation has recently updated its recommendations in this area20.
Another interesting trend was the presence of active cancer in seven patients, six of whom had ischaemic strokes, and one, with myeloma, who had haemorrhage. Malignancy has been associated with an increased risk of both ischaemic and haemorrhagic strokes21, and in-hospital mortality from stroke appears to be higher in these patients22. While this may in part be explained by shared risk factors such as smoking and obesity, there are a number of other proposed mechanisms for the pathogenesis of stroke in cancer23. This raises the issue of screening for an undiagnosed cancer in patients who present with cryptogenic stroke, as it may be considered a sign of hypercoagulability similar to unprovoked DVT or pulmonary embolism.
Overall our study describes the patterns of mortality in modern stroke care and identifies areas for further research focus, in which improved treatments and processes of care could impact further on mortality from stroke.
Conflicts of Interest
The authors declare that there are no conflicts of interest in this paper.
Correspondence:
Maeve D’Alton, Department of Age-related Healthcare, Adelaide & Meath Hospital, Tallaght, Dublin 24, Ireland.
Email: [email protected]
Reference
1. Central Statistics Office – Vital Statistics Yearly Summary 2014 www.cso.ie
2. GraphPad Prism version 7 for Mac, GraphPad Software, La Jolla California USA, www.graphpad.com
3. McCormack P, Howard D, McMahon A, Collins DR, McConaghy D, O’Neill D. An Acute Stroke Service: Potential to Improve Patient Outcome Without Increasing Length of Stay, Irish Medical Journal 2000:93(3); 84-86
4. Sentinel Stroke National Audit Programme (SSNAP) Annual Results Portfolio April 2013 – March 2014, Royal College of Physicians
5. Rudd AG, Irwin P, Rutledge Z, Lowe D, Wade DT, Pearson M. Regional variations in stroke care in England, Wales and Northern Ireland: results from the National Sentinel Audit of Stroke. Clinical Rehabilitation 2001; 15:562-572
6. National Healthcare Quality reporting System First Annual report, Department of Health http://health.gov.ie/blog/publications/national-healthcare-quality-reporting-system/ (5 March 2015, accessed 27 October 2016)
7. McElwaine P, McCormack J, Harbison J on behalf of the National Stroke Programme Audit Sterring Group. Irish Heart Foundation/HSE National Stroke Audit 2015, December 2015. https://hse.ie/eng/about/Who/clinical/natclinprog/strokeprogramme/NationalStrokeAudit2015.pdf (accessed 27 October 2016)
8. Hofmeijer J, Kappelle LJ, Amelink GJ, van Gijn J, van der Worp HB for the HAMLET investigators. Surgical decompression for space-occupying cerebral infarction (the Hemicraniectomy After Middle Cerebral Artery infarction with Life-threatening Edema Trial [HAMLET]): a multicenter, open, randomized trial. Lancet Neurology 2009; 8: 326-33. DOI: 10.1016/51474-4422)09)70047-X
9. Vahedi K, Vicaut E, Mateo J, Kurtz A, Orabi M, Guichard J, Boutron C, Couvreur G, Rouanet F, Touzé E, Guillon B, Carpentier A, Yelnik A, George B, Payen D, Bousser M on behalf of the DECIMAL investigators. Sequential-Design, Multicenter, Randomized, Controlled Trial of Early Decompressive Craniectomy in Malignant Middle Cerebral Artery Infarction (DECIMAL Trial). Stroke 2007;38:2506-2517. DOI:10.1161/STROKEAHA.107.485235
10. Juttler E, Unterberg A, Woitzik J, Bosel J, Amiri H, Sakowitz OW, Gondan M, Schiller P, Limprecht R, Luntz S, Schneider H, Pinzer T, hobohm C, Meixenberger J, Hacke W for the DESTINY II investigators. Hemicraniectomy in Older Patients with Extensive Middle-Cerebral-Artery Stroke. N Engl J Med 2014; 370:1091-1100. DOI: 10.1056/NEJMoa1311
11. Mendelow AD, Gregson BA, Fernandes HM Murray GD, Teasdale GM, Hope DT, Karimi A, Shaw MDM, Barer DH for the STICH investigators. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the International Surgical Trial in Intracerebral Haemorrhage (STICH): a randomized trial. Lancet 2005;365 (9457): 387-97
12. Mayer SA, Brun NC, Begtrup K, Broderick J, Davis S, Diringer MN, Skolnick BE, Steiner T. Efficacy and Safety of Recombinant Factor VII for Acute Intracerebral Haemorrhage. N Engl J Med 2008; 358:2127-2137. DOI: 10.1056/NEJMoa0707534
13. Tranexamic acid for hyperacute primary intracerebral haemorrhage (TICH-2). www.tich-2.org
14. Bereczki D, Fekete I, Prado GF, Liu M. Mannitol for acute stroke. Cochrane Database Syst Rev. 2007 Jul 18;(3):CD001153.
15. Wang X, Arima H, Yang J, Zhang S, Wu Guojun, Woodward M, Munoz-Venturelli P, Lavados PM, Stapf C, Robinson T, Heeley E, Delcourt C, Lindley RI, Parsons M, Chalmers J, Anderson CS; INTERACT2 Investigators. Mannitol and Outcome in Intracerebral Hemorrhage: Propensity Score and Multivariable Intensive Blood Pressure Reduction in Acute Cerebral Hemorrhage Trial 2 Results. Stroke 2015;46(10):2762-7. doi: 10.1161/STROKEAHA.115.009357.
16. Chamorro A, Dirnagl U, Urra X, Planas AM. Neuroprotection in acute stroke: targeting excitotoxicity, oxidative and nitrosative stress, and inflammation. Lancet Neurol. 2016;15(8):869
17. Hemmen TM, Raman R, Guluma KZ, Meyer BC, Gomes JA, Cruz-Flores S, Wijman CA, Rapp KS, Grotta JC, Lyden PD; ICTuS-L Investigators. Intravenous thrombolysis plus hypothermia for acute treatment of ischaemic stroke (ICTuS-L): final results. Stroke 2010 Oct;41(10):2265-70. DOI 10.1161/STROKEAHA.110.592295
18. Martino R, Foley N, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke 2005 Dec;36(12):2756-63. DOI: 10.1161/01.STR.0000190056.76543.eb
19. Hannon N, Callaly E, Moore A, Ní Chróinín D, Sheehan O, Marnane M, Merwick A, Kyne L, Duggan J, McCormack PME, Dolan E, Crispino-O’Connell G, Harris D, Horgan G, Williams D, Kelly PJ. Improved Late Survival and Disability After Stroke With therapeutic Anticoagulation for Atrial Fibrillation: A Population Study. Stroke 2011;42:2503-2508. DOI: 10.1161/STROKEAHA.110.602235
20. Paciaroni M, Agnelli G, Falocci N, Caso V, Becattini C, Marcheselli S, Rueckert C, Pezzini A, Poli L, Padovani A, Csiba L, Szabó L, Sohn SI, Tassinari T, Abdul-Rahim AH, Michel P, Cordier M, Vanacker P, Remillard S, Alberti A, Venti M, Scoditti U, Denti L, Orlandi G, Chiti A, Gialdini G, Bovi P, Carletti M, Rigatelli A, Putaala J, Tatlisumak T, Masotti L, Lorenzini G, Tassi R, Guideri F, Martini G, Tsivgoulis G, Vadikolias K, Liantinioti C, Corea F, Del Sette M, Ageno W, De Lodovici ML, Bono G, Baldi A, D’Anna S, Sacco S, Carolei A, Tiseo C, Acciarresi M, D’Amore C, Imberti D, Zabzuni D, Doronin B, Volodina V, Consoli D, Galati F, Pieroni A, Toni D, Monaco S, Barnoello MM, Barlinn K, Pallesen LP, Kepplinger J, Bodechtel U, Gerber J, Deleu D, Melikyan G, Ibrahim F, Akhtar N, Mosconi MG, Bubba V, Silvestri I, Lees KR. Early Recurrence and Cerebral Bleeding in Patients With Acute Ischaemic Stroke and Atrial Fibrillation: Effect of Anticoagulation and Its Timing: The RAF Study. Stroke 2015 Aug;46(8):2175-82. DOI: 10.1161/STROKEAHA.115.008891
21. Zoller B, Ji J, Sundquist J, Sundquist K. Risk of haemorrhagic and ischaemic stroke in patients with cancer: a nationwide follow-up study from Sweden. Eur J Cancer 2012 Aug;48(12):1875-83. DOI: 10.1016/j.ejca.2012.01.005
22. Kneihsl M, Enzinger C, Wunsch G, Khalil M, Urbanic-Purkart T, Payer F, Niederkorn K, Fazekas F, Gattringer T. Poor short-term outcome in patients with ischaemic stroke and active cancer. J Neurology 2016 Jan;263 (1): 150-6. DOI: 10.1007/s00415-015-7954-6
23. Dearborn JL, Umutia VC, Zeiler SR. Stroke and cancer – A Complicated Relationship. J Neurol Transl Neurosci 2014; 2(1): 1039
(P750)
