Pelvic and acetabular trauma care in Ireland: the past, present and future.
J M Queally, B O’Daly, M Leonard, J P McElwain
Adelaide and the Meath, incorporating the National Children’s Hospital, Tallaght, Dublin 24, Ireland
Introduction
Pelvic injuries involve injury to the osseo-ligamentous ring structure of the pelvis or the acetabulum of either hip joint. They are typically caused by high-energy trauma and may be associated with significant morbidity or mortality at the time of injury due to excessive haemorrhage and associated abdominal, chest or head injuries with mortality rates of 8.6% to 19.1% reported for closed injuries and rates of up to 50% reported for open injuries1. Despite the severity of these injuries and the potential for poor long term outcomes, these injuries were managed with non-surgical treatment until the middle of the 20th century. Treatment typically involved prolonged bed rest, traction or compression devices, pelvic slings and spica casts with poor outcomes due to persistent pelvic deformity in pelvic injures and early osteoarthritis in acetabular fractures2,3. In the 1930’s, with the advent of radiography, significant progress was made in terms of understanding injury patterns, subsequent displacement and the significance of pelvic instability and deformity post injury. Along with the improved definitive management of pelvic injuries, similar progress was made with the immediate management of life-threatening haemodynamic instability and resuscitation with a significant improvement in mortality rate achieved over the past 50 years3,4. In contemporary trauma care, to ensure optimal outcomes, pelvic trauma is now considered a subspecialty practised in tertiary centres by fellowship trained specialists. Herein we describe the evolution of pelvic trauma care in Ireland over the past 30 years in an overall context of improved international paradigms of care and discuss potential future developments.
History in Ireland
Until the 1980’s, pelvic injury in Ireland was managed in many trauma centres across the country. Conservative treatment was the predominant treatment in keeping with international norms and involved bed rest, traction and non-weight-bearing until the injury was deemed healed. Operative procedures were occasionally performed in the 1970s and early 1980s in trauma centres throughout the country and consisted of external fixation or anterior pelvic plate stabilisation. The treatment paradigm shifted to more specialised operative treatment when Prof John McElwain returned from Sunnybrook hospital in Toronto having completed a trauma fellowship under the direction of Marvin Tile from 1983 to 1984. On return from fellowship, Prof McElwain commenced treating pelvic injuries at Dr Steevens hospital between 1985 and 1987 in patients referred from local units. Approximately 15 patients were treated per year at this time. Techniques employed involved plate fixation of acetabular fractures, pubic symphyseal injuries and sacral injuries. When the orthopaedic unit moved to the Meath hospital in 1987, referrals were taken on a national basis. During this time, intraoperative radiography improved considerably which facilitated the advent of percutaneous fixation of posterior pelvic injuries using sacroiliac screws. Sacral plate and bar fixation of posterior pelvic injuries in particular was superseded by percutaneous screw fixation. Satisfactory outcomes were also reported by the unit in the literature for the operative management of both acetabular and pelvic ring injuries5,6.
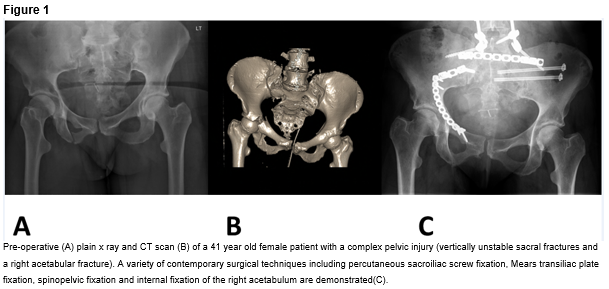
In 1998, acute services (including orthopaedic surgery) at the Meath hospital were incorporated into the new Adelaide and Meath Hospital incorporating the National Children’s Hospital in Tallaght, Dublin (AMNCH). Advances in this era included the introduction of a newer generation of implants and the increasing use of percutaneous fixation where appropriate. Spinopelvic fixation was also utilised in severe pelvic injuries that resulted in spinopelvic dissociation (Figure 1). Interventional radiology also gained prominence in the immediate management of pelvic injury with the use of angiography and embolization techniques to treat catastrophic pelvic bleeding and inferior vena caval filters to prevent fatal pulmonary embolism in high risk patients. In 2003, the unit published evidence reporting on factors associated with poor outcomes after acetabular fractures7. In a review of 180 acetabular fractures treated operatively over a 10 year period, poor functional outcomes were associated with sub-optimal reduction, complex fracture patterns, local complications and heterotopic ossification7. Further research also demonstrated that radiographic outcome poorly predicted functional outcome8.
In 2010, the unit was designated the National Centre for Pelvic and Acetabular surgery in recognition for the tertiary referral service provided by the unit over the preceding 25 years. The aim was to consolidate resources available for treating patients referred on a national basis. In particular, historically prolonged transfer times from peripheral units were hoped to be improved on. Protected trauma beds and priority intensive care beds were agreed to allow immediate transfer of patients where appropriate. In 2012, the unit reported on the long term follow-up (minimum 10 years) of 44 acetabular fractures treated surgically9. Thirteen point eight percent (two patients) had progressed to total hip replacement. Of the remaining patients, 63% reported good or excellent functional outcome. Poor functional outcome was associated with multiple concurrent injuries9. Current annual referrals requiring operative treatment are approximately 115 to 125 cases annually with referrals received on a national basis10.
Future Directions
A major challenge remains the early management of immediate catastrophic bleeding in severe pelvic injuries. Standard treatment involves instituting pelvic mechanical stability as soon as possible to reduce pelvic volume and facilitate stable clot formation11. Immediate transfer to a specialist centre should be arranged ideally within 24 hours of the injury. Definitive fixation of pelvic injuries should then occur within 72 hours of the injury. Recent developments in resuscitation include the use of the antifibrinolytic agent tranexamic acid, rapid computed tomography (CT) in the emergency department to identify sources of bleeding and early blood transfusion (as opposed to fluid resuscitation) via massive transfusion protocols12. Further management for patients who fail to respond to temporary mechanical stabilisation of the pelvis and resuscitation include angiographic embolization or surgical pelvic packing via a laparotomy13,14. The exact role for each of these techniques remains undefined, with multi-centre randomised trials required to establish protocols driven by multi-specialist care including orthopaedic surgeons, general surgeons and interventional radiologists.
Another developing area of interest is the use of percutaneous techniques in pelvic reconstruction after both pelvic and acetabular injuries. In theory, this facilitates fracture healing and reduces morbidity as the soft tissue envelope around the injured pelvic segment is largely preserved. Examples include sacroiliac screw placement for posterior pelvic ring injuries, retrograde pubic rami screws for certain anterior ring injuries, and periacetabular screw placement for the few acetabular fractures that are minimally displaced. It must be noted however, that percutaneous fixation is technically difficult and is associated with potentially significant complications due to complex pelvic anatomy. To overcome this, advanced image guided techniques including 3D fluoroscopy navigation and CT based navigation have been developed and are showing promise15.
Other challenges include those associated with providing a tertiary service in general. These include a lack of resources in the form of personnel, perioperative facilities, theatre capacity, patient transfer to the unit, access to HDU/ICU beds, access to rehabilitation and funding mechanisms underlying the entire service. In particular, timely transfer to a specialised unit is critical to avoid complications associated with delayed treatment. In terms of personnel, a multi-disciplinary team is required to manage these complex injuries including orthopaedic surgeons, theatre personnel, intensive care specialists, radiology service and rehabilitation services. Funding of the service also needs to be overhauled to ensure that appropriate funding is allocated on a per case basis following a “money follows the patient” model rather than via a traditional pre-assigned annual allocation.
Another major challenge for the future is establishing treatment guidelines based on high levels of evidence to ensure that patients receive optimal care. Currently, different practices exist in different jurisdictions regarding some aspects of treatment due to a lack of evidence to support one practice over another. For example, in early uncontrolled bleeding after severe pelvic injury, treatment by emergency pelvic packing is preferred in Europe whereas in the U.S. embolization is preferred. One of the reasons for a lack of evidence underpinning some aspects of contemporary practice is the number of patients treated in individual units is insufficient to power randomised controlled trials. This would be overcome by collaboration between multiple units both in trial design and patient recruitment.
In summary, this review describes the evolution of pelvic trauma care in Ireland over the past 30 years in tune with changing international practice. The unit has now evolved to a multi-disciplinary service with fellowship trained specialists. The paradigm of care has evolved from conservative non-operative management to operative care involving sophisticated techniques such as angiographic embolization and image-guided percutaneous fixation. Despite these advances however, significant challenges remain in place, including the emergency management of catastrophic bleeding, lack of evidence underpinning some aspects of practice and difficulties with funding and resource allocation. Solutions include multi-centre collaboration in research and the use of appropriate funding models. Our unit remains dedicated to the provision of care for these severe injuries and aims to contribute to the continued development of this subspecialty in a national and international context.
Correspondence:
Joseph M Queally, Orthopaedic Specialist Registrar, AMNCH, Dublin 24, Ireland
Email: [email protected]
Conflict of Interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical Approval
Ethical approval was not required for the preparation of this manuscript in keeping with the guidelines of our institutional ethical board
References
1. Pohlemann T, Bosch U, Gansslen A, Tscherne H. The Hannover experience in management of pelvic fractures. Clinical orthopaedics and related research 1994:69-80.
2. Henderson RC. The long-term results of nonoperatively treated major pelvic disruptions. Journal of orthopaedic trauma 1989;3:41-7.
3. Flint L, Cryer HG. Pelvic fracture: the last 50 years. The Journal of trauma 2010;69:483-8.
4. Hak DJ, Smith WR, Suzuki T. Management of hemorrhage in life-threatening pelvic fracture. The Journal of the American Academy of Orthopaedic Surgeons 2009;17:447-57.
5. Keogh P, Maher M, McElwain J. The early results of internal fixation of displaced acetabular fractures. Irish journal of medical science 1991;160:130-3.
6. O’Flanagan SJ, Fulton G, O’Beirne J, McElwain JP. Operative fixation of unstable pelvic ring injuries in polytrauma patients. Irish journal of medical science 1992;161:39-41.
7. Murphy D, Kaliszer M, Rice J, McElwain JP. Outcome after acetabular fracture. Prognostic factors and their inter-relationships. Injury 2003;34:512-7.
8. Rice J KM, Dolan M, Cox M, Khan H, McElwain JP. Comparison between clinical and radiologic outcome measures after reconstruction of acetabular fractures. J Orthop Trauma 2002;16:82-5.
9. Magill P, McGarry J, Queally JM, Morris SF, McElwain JP. Minimum ten-year follow-up of acetabular fracture fixation from the Irish tertiary referral centre. Injury 2012;43:500-4.
10. O’Neill F, Leonard M, Lui D, McElwain J, Morris S. Pelvic and acetabular fractures. Irish medical journal 2012;105:306.
11. Wong JM, Bucknill A. Fractures of the pelvic ring. Injury 2013.
12. Moran CG, Forward DP. The early management of patients with multiple injuries: an evidence-based, practical guide for the orthopaedic surgeon. The Journal of bone and joint surgery British volume 2012;94:446-53.
13. Langford JR, Burgess AR, Liporace FA, Haidukewych GJ. Pelvic fractures: part 1. Evaluation, classification, and resuscitation. The Journal of the American Academy of Orthopaedic Surgeons 2013;21:448-57.
14. Suzuki T, Smith WR, Moore EE. Pelvic packing or angiography: competitive or complementary? Injury 2009;40:343-53.
15. Stockle U, Schaser K, Konig B. Image guidance in pelvic and acetabular surgery–expectations, success and limitations. Injury 2007;38:450-62.
(P607)