Pilot evaluation of an online weight management programme
S Cawley1, S Farrell1, DG Byrne2, MJ Turner 3, B Clune4, D McCartney1
1School of Biological Sciences, Dublin Institute of Technology, Kevin St., Dublin 8, Ireland;
2GEMS Directorate, St. James’s Hospital, James’s St., Dublin 8, Ireland;
3UCD Centre for Human Reproduction, Coombe Women and Infants University Hospital, Cork St., Dublin 8, Ireland;
4DIT Student Health Centre, Dublin Institute of Technology, Aungier Street, Dublin 8, Ireland.
Abstract
This intervention examined the efficacy of a six-week online weight loss programme. Students and staff of a third level institution (n=183) were recruited to the programme which provided individualised dietary advice for weight loss. Eighty-five participants (mean age 29.7 years, mean BMI 28.9kg/m2, 33% male) met the minimum inclusion criterion of logging on to the study website at least twice. All participants who completed the full six-week programme lost weight (n=31), with significant reductions in mean weight (2.8kg), BMI (0.9kg/m2) and waist circumference (4.1cm) observed between the start and end of the programme (all P<0.001). Among “completers”, males lost more weight than females (4.2kg vs. 1.9kg, P=0.004). One in four completers lost >5% of their bodyweight, with reductions in biscuit and alcohol consumption being most predictive of weight loss. These findings suggest that individualised online dietary advice is effective in achieving short-term weight loss, especially in males.
Introduction
Latest research from Ireland reveals that 37% of Irish adults are overweight with a further 23% classified as obese1. Weight loss interventions are traditionally held “in-person”, but may fail to engage those who prefer a more anonymous means of receiving weight loss advice2. Studies evaluating online weight management programmes show that they can achieve successful weight loss outcomes, commending them as a potentially cost-effective way of targeting obesity3-9. This study investigated whether participation in a six-week online dietary intervention programme was associated with significant short-term weight loss. The dietary and lifestyle changes most associated with successful weight loss, as well as participant attrition rates were also investigated.
Methods
A convenience sample of 183 staff and students of the Dublin Institute of Technology (DIT) were recruited in February 2013, with subjects who were pregnant excluded from the study. Informed written consent was obtained from all participants at their initial baseline appointment. Participants were measured in light clothing, without shoes, jackets or any heavy items in their pockets. Body weight was measured to the nearest 0.2 kg using a calibrated Seca Mechanical Floor Scales, model 731 (Seca Ltd., Birmingham, UK), while height was measured to the nearest 0.5cm using a “Leicester Height Measure” stadiometer (Chasmore’s Ltd., London, UK). Waist circumference was measured at the mid-point between the lower rib margin and the supra-iliac crest on the mid-axillary line using a 150cm measuring tape (Korbond Industries Ltd., Grantham, UK) as described previously10. At the initial appointment, participants were shown how to login to the online application, register an account and enter their anthropometric and health behavioural data. Physical activity level (PAL) was estimated using a six-point relative scale11, while the dietary assessment comprised 31 questions concerning participants’ eating pattern and their current intake of fruit and vegetables; high fibre breakfast cereals; starchy carbohydrates; meat and meat products; sugar-sweetened foods and drinks; dairy products; fatty foods and alcohol. Upon completion of the online dietary assessment, the application generated an “assessment report” outlining the overall quality of the participant’s diet and highlighting two explicit, personalised dietary goals to be implemented.
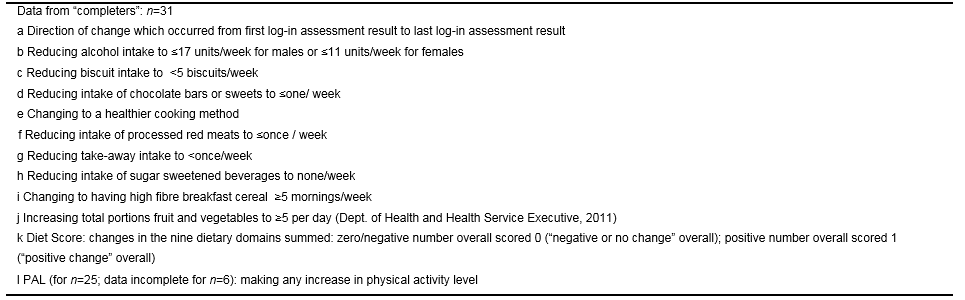
Each week, participants received a motivational e-mail inviting them to login again and re-take their assessments. On the basis of their updated answers, the application generated two new personalised dietary goals for implementation. An initial and final diet score was generated for each respondent who completed the programme. These were derived by determining whether the participant reported a “positive” change in behaviour (scored 1) or a “negative” change in behaviour (scored -1) in relation to each of the ten dietary and physical activity domains under examination. A positive change reflected a change in participant behaviour towards better compliance with national dietary guidelines in that domain. Where dietary behaviour remained unchanged at the conclusion of the six week programme, participants received a score of 0 for that domain.
The overall dietary change score was then computed for each participant, by summing their dietary change scores (1, 0 or -1) from each of the ten individual dietary and physical activity domains. At the end of the six-week online programme, repeat anthropometric measurements were taken. Using PASW v.20.0 (©IBM Corp., Armonk, New York), independent samples t-tests were used to compare the characteristics of the full baseline cohort against those of the group who completed the programme; and to assess differences in mean weight change between groups reporting differing changes in dietary behaviours. Paired t-tests were used to assess the significance of weight and waist circumference changes amongst those completing the six-week programme. Binary logistic regression analyses were performed to identify factors associated with the achievement of ≥3% weight loss over the course of the programme. A significance level of P<0.05 was cited for all statistical analyses.
Results
One hundred and eighty-three participants were recruited to the pilot online programme. Ninety eight participants (53.6%) did not meet the inclusion criterion of logging onto the online application at least twice over the six-week programme and were excluded from further analysis.
Eighty-five subjects (46.4% of the initial population) met this minimum inclusion criterion. These 85 participants comprised the baseline cohort and were predominantly overweight or obese (45% overweight and 32% obese). Thirty-five participants (19.1%) returned to be re-weighed at the end of the six-week programme. Of these 35 “completers”, four were excluded; three because they failed to meet the minimum inclusion criterion of logging in two times or more, and one because of incomplete data. This yielded a final sample of 31 programme “completers”.
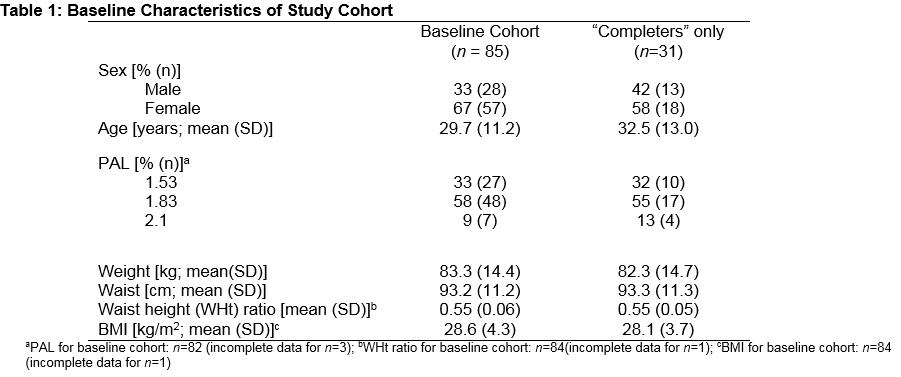
The attrition rate from the original one hundred and eighty-three participants recruited was 83%. The attrition rate from the baseline cohort of 85 participants who logged-in twice or more was 64%. The completers did not differ from the total baseline population in terms of their age, gender, physical activity or bodyweight (Table 1).
Amongst completers (n=31), significant declines in mean bodyweight (2.8kg); BMI (0.9kg/m2); waist circumference (4.1cm) and waist:height ratio (0.04) were observed between baseline and the end of the six-week programme (all P<0.001) (Table 2). Twenty-six per cent of completers (n=8; 5 male, 3 female) achieved ≥5% weight loss during the programme, while 55% of completers (n=17; 9 male, 8 female) achieved ≥3% weight loss.
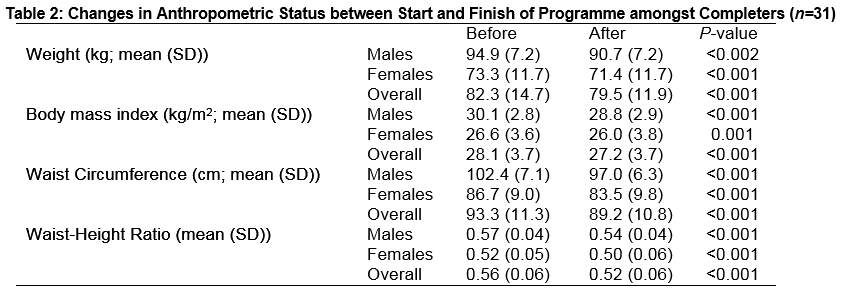
Mean weight loss was greater in males than females (4.2 (±2.5) kg versus 1.9 (±1.5) kg; P=0.004). Mean percentage initial bodyweight loss tended to be greater in males than in females (4.4 (±2.6) % versus 2.6 (±2.1) %; P=0.052). Mean reduction in waist circumference among males compared to females was 5.4 (±2.8) cm versus 3.2 (±2.5) cm, but again, this did not reach statistical significance (P=0.07).
Those who made a “positive change” in their biscuit consumption achieved a significantly greater percentage reduction in initial body weight (5.1 (± 3.1) %) than those who made a “negative or no change” (2.9 (±2.0) %; P=0.03) (Table 3).
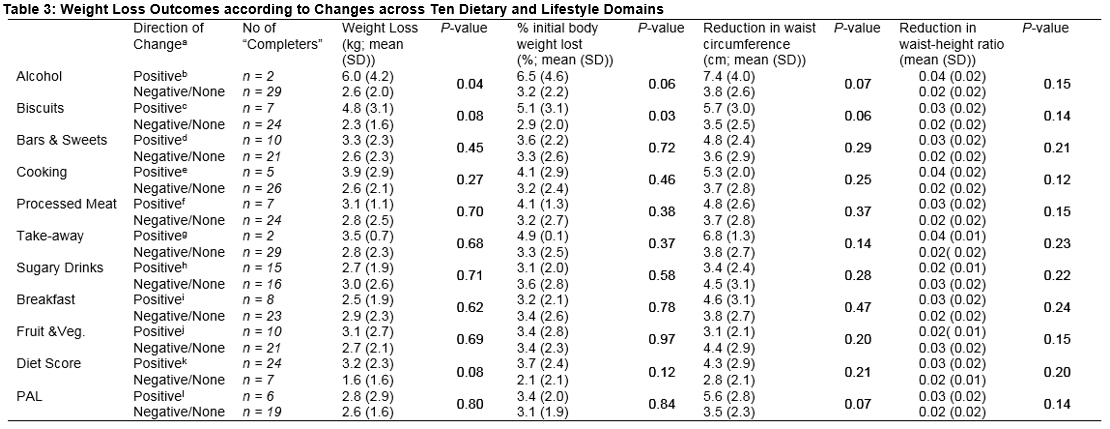
Those who made a “positive change” in biscuit intake also lost 2kg more weight and approximately 2cm more from their waist circumference than those who had a “negative or no change” in this domain, although these differences did not reach statistical significance (P=0.08 and P=0.06 respectively).
A “positive change” in alcohol consumption (i.e. reduced intake) was associated with greater weight loss than making “negative or no change” in alcohol consumption (P=0.04). Mean percentage body weight lost (6.5 (±4.6) % versus 3.2 (±2.2) %) and mean waist circumference reduction (7.4 (±4.0) cm versus 3.8 (±2.6) cm) also tended to be greater among those who made a “positive” change in alcohol consumption, than among those who did not. However, these differences did not reach statistical significance (P=0.06 and P=0.07 respectively).
In absolute terms, reduction in waist circumference tended to be greater amongst those who made a “positive change” in PAL (5.6 (± 2.8) cm) compared to those who made a “negative or no change” (3.5 (±2.3) cm); while weight loss tended to be greater in those with a “positive change” in overall diet score (3.2 (±2.3) kg) versus those with a “negative or no change” on this index (1.6 (±1.6) kg. Neither of these trends reached statistical significance however (P=0.07 and P=0.08 respectively).
In a binary logistic regression model containing six independent variables (gender, change in alcohol consumption, change in biscuit consumption, change in consumption of chocolate bars and sweets, change in PAL and change in cooking method), no variable made a unique independent contribution to the likelihood of losing ≥3% body weight. The model as a whole explained between 14.4% (Cox & Snell R2) and 19.2% (Nagelkerke R2) of the variance in likelihood of achieving ≥3% weight loss.
Discussion
This six-week online weight loss programme achieved statistically significant weight loss amongst those who completed it. While weight loss with this online programme falls below the average of 4-8kg 6,12,13 achieved with other online programmes incorporating a behavioural change element, it is also of significantly shorter duration than these other programmes. The proportion of “completer” participants who achieved clinically significant (≥ 5%) weight loss is in the mid-range of other more traditional “in-person” interventions studied in the UK (26% for the current study versus 15.7% in the general practitioner (GP) group, 18% in the National Health Service (NHS) group-based community weight loss programme “Size Down” and 46% in Weight Watchers)14. This is an important finding when one considers the high cost associated with such “in-person” programmes3. In the current study, male “completers” achieved greater weight loss than females, and lost an average of 5.4 cm from their waist circumference. Sixty-three per cent of males who completed the programme achieved ≥5% weight loss. While it must be noted that they began at a higher baseline weight compared to female participants, these results are nonetheless promising given that far fewer males than females engage in “in-person” weight loss trials2,14. The flexibility of the current programme may have contributed to its success amongst male participants, who in other studies describe time constraints as a prominent barrier to weight loss15.
The current study showed that those who reduced their biscuit consumption achieved greater percentage weight loss than those who didn’t. Data from the North/South Ireland Food Consumption Survey (NSIFCS) indicated that for each 1g/day increase in consumption of biscuits, cakes and pastries, the odds ratio (OR) for being obese was 1.0510 making it a key target food group for weight loss interventions.
The current study also showed that those who reduced alcohol consumption below the guidelines set by the Department of Health (DoH)16 (“positive change”) achieved greater weight loss than those who had a negative or no change. Heavy drinking is associated with increased prevalence of weight gain and obesity17,18. While a “positive change” in physical activity level (PAL) did not predict differences in weight loss or waist circumference reduction; those who made a “positive change” had a mean reduction in waist circumference which in absolute terms was more than 2cm greater than those who didn’t. This is important because it is abdominal adiposity which confers the greatest risk to human health18.
The current programme compares unfavourably with other online weight loss programmes which report attrition rates of between 20-30%. Many participants cited work commitments or exam pressures as impediments to completing the programme. It is also possible that participants who may have over-indulged during their Easter holidays did not want to return to be re-weighed so soon after this break21. Additionally, 52% of the baseline cohort were aged 18-25 years, with young age previously highlighted as a predictor of attrition in adult weight loss programmes22.
Results in this study are for initial weight loss only, and therefore the ability of this programme to produce long-term weight loss remains to be demonstrated. The high attrition rates and high percentage of individuals who didn’t log-in again after their initial visit significantly reduced the power of this study, making definitive statistical conclusions elusive in many cases. Other limitations include the self-selected, convenience sampling approach used, the absence of a control population and the relatively homogenous nature of this educated sample population. Nonetheless, the findings of the current study suggest that this six-week online weight management programme results in significant reductions in weight, BMI, waist circumference and waist:height ratio among those who complete it. Males achieved significantly better weight loss outcomes than females, and the proportion of male participants was greater than that observed for more traditional “in-person” programmes. These findings suggest that this tool may be especially effective for the delivery of weight loss advice to males.
Author statements
Correspondence: Dr. Daniel McCartney, School of Biological Sciences, DIT Kevin Street, Kevin St., Dublin 8, Ireland
Email Address: [email protected]
Daniel McCartney developed the online weight loss programme and is the proprietary owner of this technology and the intellectual property embedded in it.
Acknowledgements
We acknowledge with gratitude the participation of the staff and students of Dublin Institute of Technology who participated in this study, and the assistance of the DIT Student Health Centre, particularly Barbara O’Connell, Louise O’Donnell and Gillian Mansfield in conducting the study.
Conflict of Interest:
The authors declare that they have no conflict of interest.
References
1. Department of Health. The Healthy Ireland Survey 2015 – Summary of Findings. Dublin: the Stationery Office; 2015. (Internet: http://health.gov.ie/wp-content/uploads/2015/10/Healthy-Ireland-Survey-2015-Summary-of-Findings.pdf - accessed 9th February 2016)
2. Pagoto SL, Schneider KL, Oleski JL, Luciani JM, Bodenlos JS, Whited MC. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity (Silver Spring). 2011; 20:1234–9.
3. Krukowski RA, Tilford JM, Harvey-Berino J, West DS. Comparing Behavioral Weight Loss Modalities: Incremental Cost-Effectiveness of an Internet-based Versus an In-Person Condition. Obesity (Silver Spring). 2011; 19:1629–1635.
4. McConnon A, Kirk SFL, J Cockroft JE, Harvey EL, Greenwood DC, Thomas JD, Ransley JK, Bojke L. The Internet for weight control in an obese sample: results of a randomised controlled trial. BMC Health Services Research. 2007; 7:206.
5. Womble LG, Wadden TA, McGuckin BG, Sargent SL, Rothman RA, Krauthamer-Ewing ES. A randomized controlled trial of a commercial internet weight loss program. Obesity Research. 2004; 12:1011–8.
6. Tate DF, Wing RR, Winett RA. Using Internet technology to deliver a behavioral weight loss program. 2001; 285:1172–7.
7. Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an Internet weight loss program. Archives of Internal Medicine. 2006; 166:1620–5.
8. Gold BC, Burke S, Pintauro S, Buzzell P, Harvey-Berino J. Weight loss on the web: A pilot study comparing a structured behavioral intervention to a commercial program. Obesity (Silver Spring). 2007; 15:155–64.
9. Rothert K, Strecher VJ, Doyle LA, Caplan WM,Joyce JS, Jimison HB, Karm LM, Mims AD, Roth MA. Diet and Physical Activity Web-based Weight Management Programs in an Integrated Health Care Setting: A Randomized, Controlled Trial. Obesity. 2006; 14:266–272.
10. McCarthy SN, Harrington KE, Kiely M, Flynn A,Robson PJ, Livingstone MB, Gibney MJ. Analyses of the anthropometric data from the North/South Ireland Food Consumption Survey. Public Health Nutr. 2001; 4:1099-106.
11. Food and Agricultural Organisation/World Health Organisation/United Nations University. Human Energy Requirements. Report of a Joint FAO/WHO/UNU Expert Consultation. Rome: Food and Agricultural Organisation, 2001.
12. Polzien KM, Jakicic JM, Tate DF, Otto AD. The efficacy of a technology-based system in a short-term behavioral weight loss intervention. Obesity (Silver Spring). 2001; 15:825–30.
13. Micco N, Gold B, Buzzell P, Leonard H, Pintauro S, Harvey-Berino J. Minimal in-person support as an adjunct to internet obesity treatment. Annals of Behavioral Medicine. 2001; 33:49–56.
14. Jolly K, Lewis A,Beach J, Denley J, Adab P, Deeks JJ, Daley A, Aveyard P. Comparison of range of commercial or primary care led weight reduction programmes with minimal intervention control for weight loss in obesity: LightenUp randomised controlled trial. BMJ. 2011; 343:6500–d6500.
15. Sabinsky MS, Toft U, Raben A, Holm L. Overweight men’s motivations and perceived barriers towards weight loss. European Journal of Clinical Nutrition. 2007; 61:526–31.
16. Department of Health. Your Guide to Healthy Eating Using the Food Pyramid for Adults and Children over 5 years of age, 2012. (Internet: http://health.gov.ie/wp-content/uploads/2014/03/YourGuide_HealthyEating_FoodPyramid.pdf - accessed 9th February 2016).
17. Wannamethee SG, Shaper AG & Whincup PH. Alcohol and adiposity: effects of quantity and type of drink and time relation with meals. International Journal of Obesity. 2005; 29:1436–44.
18. Arif AA, Rohrer JE. Patterns of alcohol drinking and its association with obesity: data from the Third National Health and Nutrition Examination Survey, 1988-1994. BMC Public Health. 2005; 5:126.
19. Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a randomized trial. JAMA. 2003; 289:1833–6.
20. Webber KH, Tate DF, Bowling MJ. A randomized comparison of two motivationally enhanced Internet behavioral weight loss programs. Behaviour Research and Therapy. 2008; 46:1090–5.
21. Greenberg I, Stampfer MJ, Schwarzfuchs D, Shai I; DIRECT Group. Adherence and success in long-term weight loss diets: the dietary intervention randomized controlled trial (DIRECT). Journal of the American College of Nutrition. 2009; 28:159–68.
22. Gokee-LaRose J, Gorin AA,Raynor HA, Laska MN, Jeffery RW, Levy RL, Wing RR. Are standard behavioral weight loss programs effective for young adults? International Journal of Obesity. 2009; 33:1374–80.