Saving Blood and Reducing Costs: Updating Blood Transfusion Practice in Lower Limb Arthroplasty
Fenelon C1, Galbraith JG1, Kearsley R2, Motherway C2, Condon F1, Lenehan B1
1 Department of Orthopaedic Surgery, University Hospital Limerick, Limerick, Ireland
2 Department of Anaesthesia, University Hospital Limerick, Limerick, Ireland
Abstract
Aim
Our aim was to quantify blood transfusion rates in lower limb arthroplasty following the introduction of a multimodal enhanced recovery programme (ERP). We then sought to update the maximum surgical blood ordering schedule (MSBOS) and calculate cost savings achieved.
Methods
A retrospective cohort study was conducted of all patients who required blood transfusion following primary and revision total hip and knee arthroplasty in 2012 and 2015. A multimodal ERP was introduced in 2015. Cost savings were calculated following the introduction of a new MSBOS.
Results
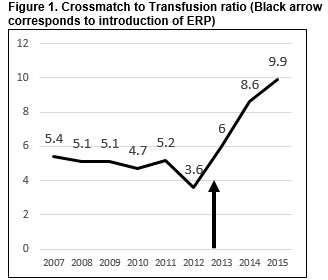
During the two-year study period 1467 lower limb arthroplasty procedures were performed. The cross-match to transfusion ratio was 3.6:1 in 2012 and 9.9:1 in 2015. The updated MSBOS resulted in a 46% reduction of cross-matched blood and savings of €54,375 per annum.
Conclusion
Improved perioperative management in lower limb arthroplasty has reduced blood transfusion rates. Updating blood transfusion practice can result in considerable savings in blood, resources and costs.
Introduction
Blood transfusion rates in lower limb arthroplasty have fallen as a result of a number of improvements in the perioperative period. Enhanced recovery programmes (ERPs), use of tranexamic acid and multimodal blood management programmes have helped in reducing the requirement. However, despite these reductions large numbers of unnecessary blood tests and blood continues to be crossmatched. Blood is valuable and limited resource that is regularly in short supply and reliant on the donations of volunteers. In Ireland 3,000 blood donors are needed each week, however, only three percent of eligible Irish people donate blood to provide for a population of four million1. Enhanced recovery programmes were introduced in the 1990s and have now been adopted across a number of surgical specialties. They have reduced length of stay and costs and improved patient satisfaction and outcomes2-5. Tranexamic acid has been one of the major contributors to the reduced need for blood transfusion in lower limb arthroplasty. Numerous studies have shown it to be both safe and effective6,7.
As healthcare costs continue to rise, efficiencies and cost savings have now become an area of considerable focus. However, it is important that cost savings do not come at the expense of patient safety. Blood is a valuable resource but also a costly resource to collect, prepare and transfuse. The average total cost of transfusing one unit of blood is estimated to be 170 sterling to 1000 dollars including processing and staffing costs8,9. Most centres utilise a maximum surgical blood ordering schedule (MSBOS) that provides a recommendation on the number of units of blood that should be cross-matched preoperatively. With changes in practice this must be regularly updated. The aim of our study was to quantify blood transfusion rates in lower limb arthroplasty following the introduction of an ERP. We then sought to update the maximum surgical blood ordering schedule (MSBOS) and assess the savings achieved.
Methods
A retrospective cohort study was conducted of all patients who required blood transfusion following primary and revision Total Hip Arthroplasty (THA) and Total Knee Arthroplasty (TKA) in our institution in 2012 and 2015. An ERP was introduced in a phased basis during 2013 and 2014, so comparison was made between 2012 (pre-ERP) and 2015 (post ERP). Procedures were performed in a dedicated orthopaedic hospital located 17 kilometres from the tertiary referral centre for the region where blood transfusion services are provided. Data was collected and cross referenced from the hospital blood transfusion database, patient medical records and laboratory databases. Baseline demographic information, pre-operative and pre transfusion haemoglobin values, type of anaesthesia, use of tranexamic acid, length of surgery, blood loss, intraoperative transfusion, perioperative transfusion defined as transfusion occurring within 6 hours of surgery, time from surgery to transfusion and number of units of red cell concentrate transfused were recorded. Statistical analysis was performed using SPSS 20.
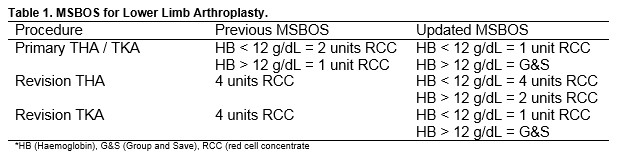
A multimodal enhanced recovery programme was applied for all procedures in 2015. This involved preoperative assessment, intravenous administration preoperatively of tranexamic acid and cefuroxime, use of spinal anaesthesia where possible and post-operative anticoagulation with prophylactic enoxaparin for 48 hours followed by rivaroxaban. Patients were mobilised as soon as possible following surgery. TKA was performed with the use of a tourniquet. Drains were not used. A GXM was taken on the morning of the procedure. For primary arthroplasty one to two units of blood were cross-matched (two units if the preoperative haemoglobin was <12g/dL) while for revision arthroplasty four units of blood were cross-matched regardless of preoperative haemoglobin [Table 1]. The haemoglobin level was routinely measured on post-operative day two. In certain cases, if blood loss was thought to be high it was taken earlier. The decision to transfuse was made by the primary surgical team. Blood transfusion was administered according to hospital guidelines if the haemoglobin level was <8 g/dL and <10 g/dL to patients with cardiovascular disease.
After consultation with the blood transfusion laboratory and haematology department the MSBOS was updated in 2016 [Table 1] and introduced in October 2016. The cost of performing one group and crossmatch (€75.00) was provided by the Blood transfusion laboratory. Using the number of procedures performed in 2015 the maximum possible number of cross-matched units of blood was calculated for the previous MSBOS and updated MSBOS. The potential saving per annum was then calculated.
Results
A total of 1467 lower limb arthroplasty procedures were performed during the two-year study period, 740 in 2012 and 727 in 2015. The number of units transfused in 2012 and 2015 was 386 units (172 patients) and 95 units (52 patients) respectively. The crossmatch to transfusion ratio (CT ratio) in 2012 was 3.6:1 and in 2015 had risen to 9.9:1 [Figure 1]. This rise was due to the same number of units of blood being cross-matched in 2015 but a reduction in the number of units of blood being transfused. The mean age in 2012 was 70 years (SD 9.9 years) and in 2015 70.7 years (SD 9.8 years). There was no significant difference in gender between 2012 and 2015 with 59.9% female in 2012 compared with 67.3% in 2015 (p=0.331). Spinal anaesthesia was performed in 79.5% of patients in 2015 compared with 84.8% in 2012. The number of intra operative blood transfusions fell from 26 to 7 between 2012 and 2015. While the number of peri-operative transfusion within six hours of surgery fell from 37 to 5. Tranexamic acid was given to 65% of patients in 2015. Overall there was a significant difference in blood loss between the two time periods, 585mls compared with 377 mls (p=0.034).
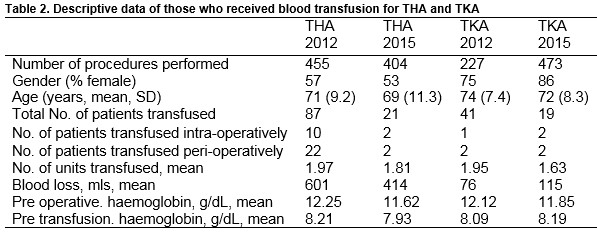
THA group
455 and 404 patients underwent primary THA in 2012 and 2015, respectively [Table 2]. In 2012, 87 patients (19.1%) were transfused while 21 patients (5.2%) were transfused in 2015. Ten patients required blood intra-operatively in 2012 compared with two in 2015 and 22 patients were given blood peri-operatively compared with two patients in 2015. The average intraoperative blood loss in primary THA fell from 601 mls to 414 mls between 2012 and 2015. The mean number of units transfused for primary THA in 2012 was 1.97 and 1.81 in 2015.
TKA group
In 2012, 227 patients underwent primary TKA compared with 273 patients in 2015 [Table 2]. A blood transfusion was required in 41 patients (18%) in 2012 and 19 patients (7%) in 2015. One patient was transfused intra operatively and two patients peri-operatively in 2012 compared with two patients transfused both intra and peri-operatively in 2015. The mean number of units transfused for primary TKA was 1.95 and 1.63 respectively for 2012 and 2015. The average intraoperative blood loss in primary TKA was 76 mls in 2012 and 115 mls in 2015. The reason for this rise was due to one patient who had an intraoperative blood loss of 900mls. If this patient was excluded the average intraoperative blood loss in 2015 fell to 68mls.
Cost Analysis
Using the previous MSBOS the maximum possible number of cross-matched units of blood for 2015 was 1,554. Using the updated MSBOS the maximum possible number of cross-matched units was 829 cross-matched units of blood, a reduction of 46.6%. Using the cost to group and crossmatch one unit of blood of €75.00, savings of €54,375 were calculated based on if the same number of procedures were performed for the following year [Table 3].
Discussion
Blood transfusion is associated with considerable costs as a result of the numerous resources and personnel involved. As shown in other studies review of blood transfusion practices and updating the MSBOS can result in significant reductions in the number of cross-matched blood10,11. More than €54,000 per annum was saved in our study as a result of the reduction in cross-matched blood. The ratio of cross-matched to transfused blood (CT ratio) provides a simple tool to measure the efficiency of this system. In 2015 our CT ratio had risen to 9.9:1, considerably higher than that in 2012 of 3.6:1. While this is far higher than the recommended 2-3:112. These figures may be partially explained by the fact that no blood transfusion service exists on site in our institution. Despite this disproportionate cross-matching of blood was still occurring which we hope has now been addressed by the updated MSBOS.
Large numbers of studies have now been published highlighting the effectiveness and safety of tranexamic acid in reducing the need for blood transfusion in total hip and knee arthroplasty13. Introduction of tranexamic acid in our institution has helped reduce the requirement for transfusion however it is not the sole reason but likely one of the parts in a multimodal ERP. One of the incidental findings of our study found that in 2015 only 65% of patients that underwent transfusion had received tranexamic acid. This has since been addressed with the inclusion of the question “Has tranexamic acid been given?” to the surgical safety checklist. With this we hope that a future audit will show 100% compliance.
While the majority of hospitals perform a preoperative group and save in lower limb arthroplasty some, including our institution continue to routinely crossmatch blood. Some studies are now beginning to question the need for a preoperative group and save14,15. A recent retrospective study of 996 patients over a one-year period undergoing lower limb arthroplasty using a multimodal ERP reported that just one patient required blood on the day of surgery14. While the number of intraoperative transfusions given has fallen in our study (26 to 7), there is still a need for blood urgently. Studies have suggested the use of O negative blood in emergency situations where cross-matched blood is not immediately available14-16. However, even with O negative blood there is still a small risk of a transfusion reaction if the patient has atypical red cell antibodies. It is also a scarce resource found in only 6-8 % of the population17. It is important that the quest to reduce costs does not come at the expense of patient safety.
Our study is not without limitations. This study was retrospective in nature thus reliant on the records that exist. Also variations in application of the ERP exist among both surgical and anaesthetic clinicians. Our figure of cost savings is likely an underrepresentation of the actual costs as transport, administration and staffing costs were not included.
Blood transfusion requirements in lower limb arthroplasty have dropped following the introduction of a number of new perioperative measures and blood management practices. It is important that centres now review and update their blood transfusion policies to reduce the burden on the strained blood transfusion service as well as reducing costs.
Conflicts Of Interest
The authors have no conflicts of interest to declare
Correspondence
Christopher Fenelon, Department of Orthopaedic Surgery, University Hospital Limerick, Limerick, Ireland, IRL
Email: [email protected]
References
1. Irish Blood Transfusion Service: All about Blood - Did you know? Available from https://www.giveblood.ie/All_About_Blood/Did_you_Know/. Last accessed August 20 2017
2. Husted H, Jensen CM, Solgaard S, Kehlet H. Reduced length of stay following hip and knee arthroplasty in Denmark 2000-2009: from research to implementation. Arch Orthop Trauma Surg 2012;132:101-4
3. Husted H, Holm G, Jacoben S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop 2008;79:168-73
4. Larsen K, Hansen TB, Thomsen PB, Christiansen T, Soballe K. Cost-effectiveness of accelerated perioperative care and rehabilitation after total hip and knee arthroplasty. J Bone Joint Surg Am 2009;91:761-72
5. Galbraith JG, Fenelon C, Gibbons J, Kelly GA, Bennett D. Enhanced recovery in lower limb arthroplasty in the Irish setting. Ir J Med Sci. Feb 7 2017. [Epub ahead of print]
6. Wu Q, Zhang HA, Liu SL, Meng Tm Zhou X, Wang P. Is tranexamic acid clinically effective and safe to prevent blood loss in total knee arthroplasty? A met-analysis of 34 randomized controlled trials. Eur J Orthop Surg Traumatol. 2015;25(3):525-41
7. Wei Z, Liu M. The effectiveness and safety of tranexamic acid in total hip or knee arthroplasty- a meta-analysis of 2720 cases. Transfu Med. 2015;25(3):151-62
8. National Institute for Health and Clinical Excellence (2015) Costing statement: Blood transfusion – Implementing the NICE guideline on blood transfusion (NG24)
9. Kansagra A, Andrzejewski C, Krushell R, Lehman A, GReenbaum J, Visintainer P, McGirr J, Mahoney K, Cloutier D, Ehresman A, Stefan MS. Blood Management Strategies to Reduce Transfusions After Elective Lower-Extremity Joint Arthroplasty Surgeries. Am J Med Qual. 2017 Jan 1. [Epub ahead of print]
10. Rogers BA, Johnstone DJ. Audit on the efficient use of cross-matched blood in elective total hip and total knee replacement. Ann R Coll Surg Engl. 2006;88(2):199-201
11. Mahadevan D, Challand C, Clarke A, Keenan J. Maximum surgical blood ordering schedules for revision lower limb arthroplasty. Arch Orthop Trauma Surg. 2011;131(5):663-7
12. Bristish Committee for Standards in Haematology. Guidelines for the implementation of a maximum surgical blood ordering schedule. http:// http://www.bcshguidelines.com/documents/maximum_surgical_blood_order_scehdule_1990.pdf [accessed 2016 Jun 07]
13. Poeran J, Rasul R, Suzuki S, Danninger T, Mazumdar M, Opperer M, Boettner F, Memtsoudis SG. Tranexamic acid use and postoperative outcomes in patients undergoing total hip or knee arthroplasy in the United States: retrospective analysis of effectiveness and safety. BMJ 2014:12:349
14. Marson BA, Shah J, Deglurkar M. Blood transfusion in hip and knee arthroplasties: the end of the preoperative group and save? Eur H Orthop Surg Traumatol. 2015;25(5):871-5
15. Metcalfe CW, Jayatilaka ML, Cope MR. Is a preoperative group and save necessary for enhanced recovery joint replacements patients? B J Hosp Med (Lond). 2014;75(12):708-10
16. Ziali Sivardeen KA, Kalell SS, Weaver P, Chandran P. Total hip arthroplasty: to cross match or not to crossmatch an evidence based, cost effective and safe protocol. Eur J Orthop Surg Traumatol. 2008;18:107-109
17. Beckman N, Yazer M, Land K, Chesneau S, Caulfield J. Blood banks meet the paradox of Gabriel’s Horn: what are the options to maintain supply as demand decreases? Transfus Med. 2016 May 3 [Epub ahead of print]
(P730)
