Seasonal Influenza Vaccine Uptake in a Respiratory Outpatients Clinic
Rossiter A, O’Morain NR, Varghese C, Lane S.
Department of Respiratory Medicine, Tallaght Hospital, Dublin 24
Abstract
Influenza is an acute viral respiratory illness that continues to cause significant morbidity and mortality in Ireland. Despite well-established national and international guidelines1 and increased public awareness campaigns, vaccine uptake rates are well below target worldwide2. We performed an audit of influenza vaccine uptake at a Respiratory outpatient clinic in a tertiary referral centre. 54% (n=41) of patients received the annual vaccine, well below the target of 75% set by the European Centre for Disease Prevention and Control (ECDC).
Introduction
A total of 1842 confirmed hospitalised cases of influenza, and 75 notified influenza deaths were reported to the Health Protection Surveillance Centre, during the 2015/16 ‘flu season’ alone3. Patients with chronic respiratory disease, as well as those over 65 and persons who are immunosuppresed due to diesease or treatement, are strongly recommended to receive the annual influenza vaccine. Vaccination is both a safe and effective means of preventing the morbidity and mortality associated with influenza. The ECDC have set a target of 75% vaccination coverage for patients >65 years and for those with chronic illnesses4. Specialty tertiary referral centres offer a unique opportunity to educate and encourage vaccination.
Methods
All patients attending the clinic over a 2 week period in March 2016 were invited to participate in the study. Participants were invited to answer a questionnaire regarding the influenza vaccination with the guidance of their attending doctor. Patients were asked four questions to establish their vaccination status and explore their attitudes and barriers to vaccination. Inclusion criteria included a diagnosis of chronic respiratory illness. New referrals and patients without a formal diagnosis were excluded.
Results
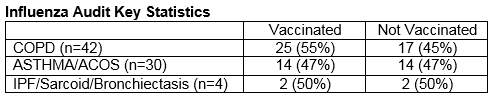
One-hundred and thirty-two patients were invited to participate in the audit, of which 14 patients (11%) declined. There were 24 (18%) new referrals and 18 patients (14%) who did not have a confirmed diagnosis who were not included. Seventy-six patients (58%) with a confirmed chronic respiratory disease were identified and included in the study. Of these, 53% (n=40) were female and 40% (n=30) were >65 years old. Of the study group, 54% (n=41) received the seasonal influenza vaccine, with the majority (80%) given the vaccine by their General Practitioner. COPD was the most common diagnosis representing 55% (n=42) of all patients, of whom 64% (n=25) were vaccinated against influenza. More males (58%) than females (50%) received the annual vaccine. The most common reason for not getting the vaccine was that the patient ‘forgot’ (41%), was wary of ‘side effects’ (12%), or was ‘unable to find the time’ (12%). Of note, 48% (n=17) of those who were not vaccinated in 2015/2016 did previously receive the annual influenza vaccine.
Discussion
Despite universal recommendation and international guidelines, influenza uptake in individuals with chronic respiratory illnesses has been poor. Estimates across Europe were found to be well below target in many European countries including Poland (8%), Sweden (11%) and in Germany (47%)5,6. Figures in the UK during the 2014/15 season show uptake rates at 72% in those participants aged over 657. Similarly, vaccination rates in Ireland during the 2010/11 season in at risk groups overall was 60%8. Well documented barriers to immunization include lack of access, beliefs and fear of injections9. While our study reports an uptake rate of 54%, we identified a significant proportion of patients not vaccinated in 2015/2016 who had previously been vaccinated. This represents a considerable cohort of patients who are indeed amenable to vaccination, and with improved awareness could contribute to increased uptake rates.
Immunization occurs primarily in the community setting. Measures to improve vaccine uptake figures previously identified include nominating a lead staff member to plan the flu campaign in each practice, setting financial targets and effective communication and education about complications of influenza illness10. There is currently no formal correspondence between specialist tertiary outpatient clinics and the community, which represents a missed opportunity to increase awareness, identify at risk patients, and improve upon vaccination uptake rates.
Despite increased awareness surrounding Influenza vaccination guidelines, only 54% (n=41) of patients with a chronic respiratory illness attending a specialty outpatient clinic were vaccinated with the seasonal influenza vaccine. This is well below the target of 75% set by the ECDC. Specialty outpatient clinics offer a unique opportunity to further patient education regarding essential vaccination. This could include enhanced correspondence to GPs in clinic letters to encourage immunisation to their patients and also prompting for the Respiratory physician to make patients aware of the need for immunisation at every outpatient appointment. To this end, we have developed a new template for patient appointment letters to include a prompt to both the patient and their local GP to consider vaccination in patients due to attend the Respiratory outpatient clinic. The audit cycle will be completed following the 2016/2017 flu season to assess whether this simple and cost effective method has any effect on increasing vaccination uptake rates.
Correspondence:
Neil Moran, Department of Respiratory Medicine, Tallaght Hospital, Dublin 24
Email: [email protected]
Conflict of Interest:
The authors report no conflict of interest
References
1. Lu P-J, O'Halloran, A., Ding, H., Srivastav, A., Williams, W.W. Uptake of Influenza Vaccination and Missed Opportunities among Adults with High-Risk Conditions, United States, 2013. American Journal of Medicine. 2016.
2. Executive HS. Influenza Vaccination 2015 [Available from: http://www.hse.ie/eng/health/immunisation/hcpinfo/guidelines/chapter11.pdf.
3. Centre HPS. Influenza Surveillance in Ireland – Weekly Report (16th-22nd May) 2016 [Available from: http://www.hpsc.ie/A-Z/Respiratory/Influenza/SeasonalInfluenza/Surveillance/InfluenzaSurveillanceReports/20152016Season/File,15688,en.pdf.
4. European Centre for Disease Prevention and Control (ECDC) http://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32009H1019&from=EN
5. Kroneman M1 vEG, John Paget W. Influenza vaccination coverage and reasons to refrain among high-risk persons in four European countries. 2006.
6. Schoefer Y ST, Raspe H , Schaefer T. Determinants of influenza and pneumococcal vaccination in patients with chronic lung diseases. 2007.
7. England PH. Seasonal influenza vaccine uptake amongst GP patients in England. Sept 2014-Jan 2015.
8. Mereckiene J1 CS, Nicoll A, Lopalco P, Noori T, Weber J, D'Ancona F, Levy-Bruhl D, Dematte L, Giambi C, Valentiner-Branth P, Stankiewicz I, Appelgren E, O Flanagan D. Seasonal influenza immunisation in Europe. Overview of recommendations and vaccination coverage for three seasons: pre-pandemic (2008/09), pandemic (2009/10) and post-pandemic (2010/11). 2014.
9. H Hollmeyer, F Hayden, A Mounts, U Buchholz. Review: interventions to increase influenza vaccination among healthcare workers in hospital. Influenza and other respiratory viruses. Volume 7, Issue 4 July 2013 Pages 604–621
10. Laura J Dexter MDT, Matthew Dexter, A Niroshan Siriwardena,, Read RC. Strategies to increase influenza vaccination rates: outcomes of a nationwide cross-sectional survey of UK general practice. 2012.
(p517)