Subtrochanteric Femur Fractures in an Irish Trauma Centre over 9 years: How the Impact of Hospital Coding on Diagnosis of Subtrochanteric Femur Fractures Leads to Inaccurate Occurrence Rates
EI Coveney, Harriz E, Gibney B, JF Quinlan
Adelaide and Meath Incorporating the National Children’s Hospital, Tallaght, Dublin 24
Abstract
Aim
Our aim was to assess the occurrence rates of subtrochanteric femur fractures in an orthopaedic tertiary referral centre and to assess the correlation of patient’s actual diagnosis with national hospital inpatient enquiry data.
Methods
Retrospective data from 2005-2014 was collected from an orthopaedic tertiary referral centre. A revision of all fractures coded subtrochanteric was performed. The plain radiograph images of each case were reviewed by two orthopaedic surgeons and one radiologist, with a reassessment performed of the fracture coding based on the AO/OTA classification system for subtrochanteric fractures.
Results
One thousand, seven hundred and one patients were admitted to our centre from January 2005 to February 2014 with hip fractures. Using ICD-10 coding, 48 fractures were coded with the diagnosis subtrochanteric femur fractures. Upon application of AO/OTA classification this was revised to 8 cases of subtrochanteric fractures over this period.
Discussion
Hospital coding of subtrochanteric fractures needs to be accurate to assess this, and all, fractures. Incorrect coding can mislead figures for this type of fracture and give incorrect diagnosis. This study has shown discrepancies between coded data and actual diagnosis. Coding improvements are essential to improve epidemiology studies of subtrochanteric fractures and for accuracy with introduction of activity based funding in to hospitals.
Introduction
Our aim was to assess the occurrence rates of subtrochanteric femur fractures in an orthopaedic tertiary referral centre and to assess the correlation of patient’s actual diagnosis with national hospital inpatient enquiry data. Subtrochanteric femur fractures have a reported incidence ranging from 1.3% to 25% of all hip fractures1-4. They are occurring with increasing incidence1 and this is projected to continue5. Subtrochanteric femur fractures have a bimodal age and gender distribution, occurring in young males from high velocity trauma, or in elderly females, from low energy falls2. There is a well-documented association between bisphosphonate use in osteoporotic elderly females and atypical subtrochanteric femur fractures6. As a result of this it is important to distinguish subtrochanteric femur fractures to intertrochanteric femur and intracapsular femur fractures or femoral shaft fractures.
With the introduction of the Irish Hip Fracture Database (IHFD) in the Republic of Ireland, there is more focus on the trends in hip fractures being seen nationwide and a renewed interest in differentiating hip fractures occurring with increasing frequency7. Also, with the move to activity based funding8, hospitals rely further on accurate record keeping and coding. This is performed through the Hospital Inpatient Enquiry System (HIPE) which is managed by the Healthcare Pricing Office (HPO)9. The HPO website reports that the influence of the HIPE system is such that it is used extensively for market research, epidemiological studies and by the Department of Health (DoH) and Health Service Executive (HSE) in the planning, provision and measurement of acute hospitals 10.
The primary aim of this study was to determine the occurrence rates of subtrochanteric femur fractures in a population presenting to a tertiary referral trauma centre in the Republic of Ireland. Our secondary aim was to assess accuracy of data collected by the trauma centre and correlation of this data with radiographic imaging. Through use of the AO/OTA classification of subtrochanteric femur fractures we wanted to determine how accurate our data collection system was. This classification system was used as there is an unacceptable degree of inter-observer variation for the Seinsheimer classification, the most commonly used system, and the AO/OTA classification system was the second most commonly used classification system for this type of fracture11.
Methods
All fractures coded subtrochanteric femur fractures ICD 10 S722, were gathered from the HIPE system in our institution over a 9-year period, from January 2005 to February 2014. From this, medical records of all cases coded subtrochanteric femur fractures were obtained to assess where in the chart that the HIPE recorded diagnosis was first documented.
A radiological review of all imaging was performed by a senior radiology specialist registrar, orthopaedic specialist registrar and senior orthopaedic registrar. Each observer reviewed images and recorded their impressions independently of one another. Using the AO/OTA classification system for subtrochanteric femur fractures a reassessment of all radiological imaging and all coded subtrochanteric femur fractures was performed. The AO/OTA classification of subtrochanteric femur fractures takes the proximal margin of the fracture line as being the inferior border of the lesser trochanter, a distal margin of three centimetre distal to the inferior border of the lesser trochanter and omits any fracture with intertrochanteric extension. Numerical classification is 32A1.1, 32B1.1 or 32C1.1. Estimation of the catchment population of our tertiary referral centre was performed using statistics provided by the Central Statistics Office of Ireland from 2011 and 2016.
Results
One thousand, seven hundred and one cases coded hip fractures by HIPE including subtrochanteric femur fractures were admitted to our institution over an 8-year period. Forty-eight cases (2.82%) in total were coded as being subtrochanteric femur fractures under ICD 10 guidelines. Mean age of these patients was 80.14 years (range 72-94, SD 8.17). The gender breakdown of these cases were as follows; 13 male, 35 female. The catchment area for the hospital was estimated at a population of 501,271 using data from the 2016 census12.
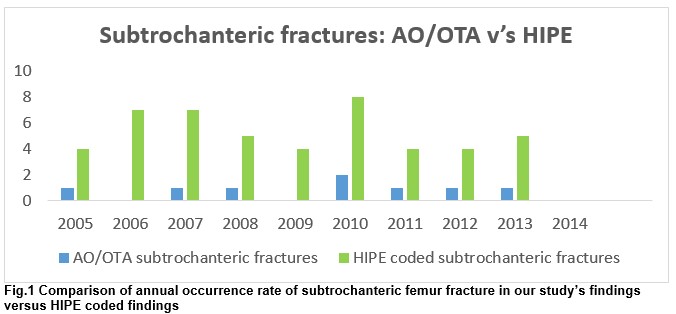
From assessing clinical notes, the diagnosis of subtrochanteric femur fracture was made on admission of the patient to hospital by a non-consultant hospital doctor (NCHD) in 31 cases. In each of these instances, this diagnosis was continuously documented throughout the inpatient stay until the patient was discharged. In the remaining cases the diagnosis was documented at discharge which was also performed by an NCHD. From review of radiological imaging, there were 8 confirmed subtrochanteric femur fractures. Each of these 8 cases were identified as subtrochanteric by the three observers. 8 cases were female and 0 male. This results with an annual rate of one cases/year and occurrence rate of 0.47% of all hip fractures that presented to our institution, over this 8 year period. Also from review of the original 48 cases, the 40 incorrectly diagnosed subtrochanteric fractures were reclassified by the observers as intertrochanteric femur fractures. Annual occurrence of subtrochanteric femur fractures was 0 to 2 cases, with breakdown in figure 1. A figure of one actual subtrochanteric femur fracture per 1.125 years was calculated.
Discussion
Subtrochanteric femur fracture rates in our institution are low with an occurrence of 8 cases over 9 years and all of female gender. Against international and national rates, our occurrence rates for subtrochanteric femur fractures remain low. The fact that our cases have been sex specific highlights that these fracture types have a well-known female predominance. Our rates of subtrochanteric factures of <1 case per over half a million population per annum reveals that these fracture types occur less frequently than what is being reported. A preliminary report from the IHFD in 2014 reported that 10% of 843 recorded hip fractures were classified as subtrochanteric fractures of the femur13. Although these figures would seem high when compared to our rates, it must be understood that the data accrued by the IHFD is derived from HIPE coded data and thus as shown, inconsistencies may arise. Also we acknowledge that the AO/OTA classification system we used is not the sole classification for this fracture type though it has been shown to have satisfactory inter and intra-observer variability.
We do note that with our study numbers being small there is potential for bias and despite the AO/OTA classification being reliable there is still potential for inter and intra-observer variability. We also recognise that as we excluded fractures extending in to the intertrochanteric region some cases may have been excluded where the fracture was unstable requiring treatment of the fracture as an AO/OTA classified subtrochanteric femur fracture. The importance of accurate coding should be emphasised to all members of clinical teams. As reported by O’ Callaghan in 2012, serious discrepancies between HIPE coded data and actual diagnosis were found on review14. From the recommendations made by that paper, further training to include clinical based work for coders and feedback for clinicians, have not been implemented in full. Clarke also reported the importance of clinician involvement in coding to improve accuracy using HIPE15. It is imperative that both junior and senior clinicians become more aware of the importance of accurate recording of data, particularly now with the introduction of activity based funding by the HSE.
A systematic review of coding in the UK by Burns reported significant improvements in coding since the introduction of payment by results16. With the roll-out of activity based funding by the HSE it is hoped that our coding practices will mirror those seen in the UK. It is important that the benefits of keeping accurate data be encouraged. An example of good quality data can be seen with the UK National Hip Fracture Database which commenced in 2009. Its 2015 report reveals that there have been increased rates of early surgery and decreased 30-day mortality rates which show the effects quality data can have in determining national figures which encourage poorly performing hospitals to improve and hence, improve patient outcomes17.
We propose that electronic coding be performed by senior clinicians at point of care to ensure accurate diagnosis is coded and that hospitals are accurately funded. We also propose that NCHD’s obtain formal training from the health care providers and hospital lead clinicians in the importance of understanding the implications of recording accurate diagnosis.
Conflict of Interest:
None
Correspondence:
EI Coveney, Adelaide and Meath Incorporating the National Children’s Hospital, Tallaght, Dublin 24
Email: [email protected]
References:
1. Wang Z, Bhattacharyya T. Trends in incidence of subtrochanteric fragility fractures and bisphosphonate use among the US elderly, 1996-2007. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research. 2011;26(3):553-60.
2. Joglekar SB, Lindvall EM, Martirosian A. Contemporary management of subtrochanteric fractures. The Orthopedic clinics of North America. 2015;46(1):21-35.
3. Adachi JD, Lyles K, Boonen S, Colon-Emeric C, Hyldstrup L, Nordsletten L, Pieper C, Su G, Bucci-Rechtweg C, Magaziner J . Subtrochanteric fractures in bisphosphonate-naive patients: results from the HORIZON-recurrent fracture trial. Calcified tissue international. 2011;89(6):427-33.
4. Huang SY, Grimsrud CD, Provus J, Hararah M, Chandra M, Ettinger B, Lo JC. The impact of subtrochanteric fracture criteria on hip fracture classification. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2012;23(2):743-50.
5. Dodds MK, Codd MB, Looney A, Mulhall KJ. Incidence of hip fracture in the Republic of Ireland and future projections: a population-based study. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2009;20(12):2105-10.
6. Park-Wyllie LY, Mamdani MM, Juurlink DN, Hawker GA, Gunraj N, Austin PC, Whelan DB, Weller PJ, Laupacis A. Bisphosphonate use and the risk of subtrochanteric or femoral shaft fractures in older women. Jama. 2011;305(8):783-9.
7. Audit NOoC. Irish Hip Fracture Database National Report 2014. National Office of Clinical Audit: National Office of Clinical Audit, Health Service Executive, Irish Institute of Trauma and Orthopaedics, Irish Gerentological Society, 2014.
8. Executive HS. Activity Based Funding Programme Implementation Plan 2015-2017. Ireland: Health Service Executive, 2015 20/05/2015. Report No.
9. Healthcare Pricing Office (HPO) HSEH. Activity in Acute Public Hospitals in Ireland Annual Report, 2014. Report. Dublin: 2015 December 2015. Report No.
10. Office HP. Available from: http://www.hpo.ie/.
11. Loizou CL, McNamara I, Ahmed K, Pryor GA, Parker MJ. Classification of subtrochanteric femoral fractures. Injury. 2010;41(7):739-45.
12. Office CS. Census 2016 Summary Results Part 1. 2017.
13. Ellanti P, Cushen B, Galbraith A, Brent L, Hurson C, Ahern E. Improving hip fracture care in ireland: a preliminary report of the irish hip fracture database. Journal of osteoporosis. 2014;2014:656357.
14. O'Callaghan A, Colgan MP, McGuigan C, Smyth F, Haider N, O'Neill S, Moore DW, Madhavan P. A critical evaluation of HIPE data. Irish medical journal. 2012;105(1):21-3.
15. Clarke B, Kennelly S, Shanley D, Hogan-Lowe D, McCormack PM. Does HIPE data capture the complexity of stroke patients in an acute hospital setting? Irish medical journal. 2010;103(1):23-4.
16. Burns EM, Rigby E, Mamidanna R, Bottle A, Aylin P, Ziprin P, Faiz OD. Systematic review of discharge coding accuracy. Journal of public health (Oxford, England). 2012;34(1):138-48.
17. Physicians RCo. National Hip Fracture Database Annual Report 2015. RCP London: Royal College Of Physicians, 2015 2015. Report No.
(P770)
