Surgical Site Infection after Caesarean Section? There Is an App for That: Results from a Feasibility Study On Costs and Benefits
C G Fawsitt1,2, S Meaney2, RA Greene2, P Corcoran2
1Bristol Medical School, University of Bristol, United Kingdom
2National Perinatal Epidemiology Centre, University College Cork, Cork, Ireland
Abstract
Surgical site infections (SSIs) are one of the most common and, yet, preventable healthcare associated infections. In Ireland, the rate of Caesarean section (CS) is increasing, while postpartum hospital stay is decreasing, adversely affecting SSI among women. There is much need to develop post-discharge surveillance which can effectively monitor, detect, and arrange treatment for affected women. The use of modern technology to survey SSI following discharge from hospital remains unexplored. We report the results of a feasibility study which investigates whether an integrated mobile application (hereafter, app) is more cost-beneficial than a stand-alone app or telephone helpline at surveying SSI following CS. We find women prefer the integrated app (47.5%; n=116/244) over the stand-alone app (8.2%; n=20/244) and telephone helpline (18.0%; 44/244), although there is no significant difference in women’s valuation of these services using willingness to pay techniques. The stand-alone app is the only cost-beneficial service due to low labour costs. Future research should employ alternative measures when evaluating the benefits of the health technology. The use of a mobile app as a mechanism for postpartum care could represent a considerable advancement towards technological health care.
Introduction
SSIs are one of the most common and, yet, preventable health-care associated infections (HCAIs)1. In Ireland, the infection affects approximately 10% of women undergoing Caesarean section (CS), or roughly 2,200 women annually2,3. The rate of CS is increasing, accounting for 30% of births in 2014 compared with 24.3% in 2003, while postpartum hospital stay is decreasing; median length of stay is estimated at three days in 2012, against five days in 20103,4. This is having an adverse effect on SSI, which can become apparent within 30 days of surgery, meaning many infections are not identified until after discharge from hospital2. This represents a significant burden on patient morbidity and mortality, and hospital costs5. SSIs prolong postpartum care where hospital costs are adversely affected by readmission with serious infections requiring surgical intervention. With reduced time spent in hospital following CS, there is much need to develop post-discharge surveillance which can effectively monitor, detect, and arrange treatment for affected women. Although there remains no widely approved mechanism to identify SSI internationally, post-discharge surveillance exists in varying forms, including self-completion questionnaires, follow-up visits, or telephone calls with a health care provider5.
Current practice in Ireland is mixed. However, women are visited in their homes by a public health nurse shortly after childbirth, where assessment of surgical wounds is undertaken among women that delivered by CS. The use of modern technology to monitor and identify SSI following discharge from hospital remains unexplored. This study considers a mobile application (hereafter, app), which may be used on a mobile device or tablet, to monitor, detect, and arrange treatment for cases of SSI among CS patients. The mobile app is compared with alternative methods of post-discharge surveillance to investigate women’s preferred service and calculate the expected costs and benefits of these services. As this is a feasibility study, we are interested in assessing the methods employed herein to inform a complete randomised controlled trial (RCT) and alongside economic evaluation, which examines the effectiveness and cost-effectiveness of the proposed interventions.
Methods
We informally compared the costs and benefits of a stand-alone app, integrated app, and telephone helpline in monitoring surgical wound post-CS in Ireland. The stand-alone app essentially represents usual care in Ireland. The app provides a range of information about CS and SSI directly to women on their phone or tablet. It allows women to record symptoms as well as temperature, heart rate and pain, among other symptoms. Based on the information recorded, the app provides advice such as to check body temperature or to contact a General Practitioner (GP). The integrated app has all the functionality of the stand-alone app, although the information recorded is checked daily by a midwife in the maternity hospital. The app allows the midwife to provide advice directly to women if necessary and instruct patients to contact their GP or return to the hospital for a consultation. The telephone helpline allows women to contact a midwife in the maternity hospital directly, where advice and instruction on appropriate courses of care can be provided.
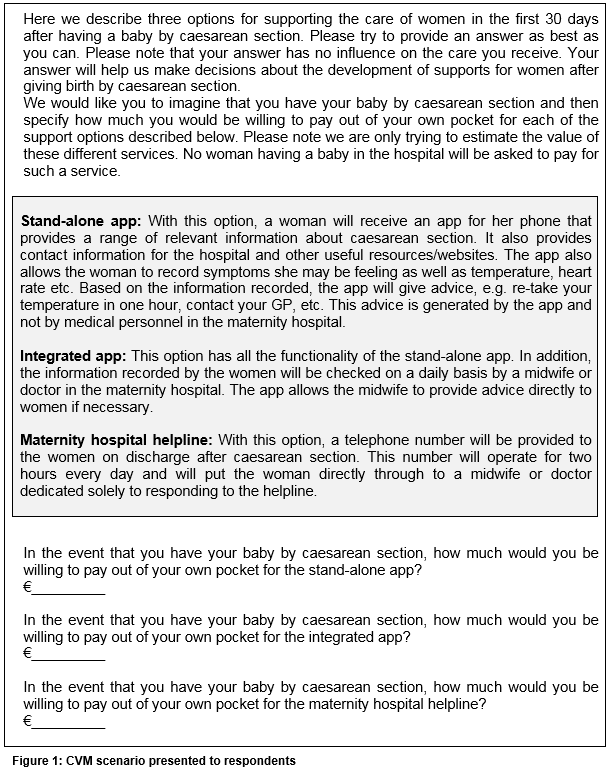
Women’s preferences for the proposed interventions are elicited using the contingent valuation method (CVM), or willingness-to-pay (WTP) method, which is a survey-based measure that captures value through simulated behaviour. In a CVM, respondents are presented with a hypothetical scenario and asked to infer how much they would be willing to pay to experience a welfare gain associated with a good or service. In this study, women are presented with the three hypothetical interventions and asked to infer how much they would be willing to pay for these services. An open-ended question is assumed (Figure 1). The payment vehicle is designed as an out-of-pocket expense given women’s expected familiarity with out-of-pocket expenses for mobile apps and telephone calls.
The CVM was distributed to 380 women in public and private antenatal clinics in Cork University Maternity Hospital (CUMH) in June 2015. Ethical approval for the study was granted by the Clinical Research Ethics Committee of the Cork Teaching Hospitals and the Division of Obstetrics and Gynaecology in CUMH. (The questionnaire can be made available by the authors on request.). The WTP data were analysed in Stata 126. The distribution of the data was explored and the data were trimmed to remove potential outliers. Descriptive statistics were used to describe both mean and median WTP values7.
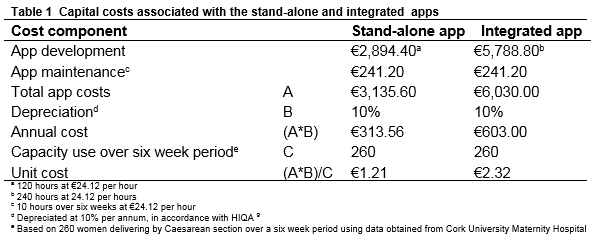
Cost estimates derived from primary data collection. We assumed a health-service perspective and collected only those service costs accruing to the Health Service Executive (HSE). Resources were valued at their opportunity costs8. All unit costs were valued at 2014 prices and expressed in Euro (€). We calculated the expected total service costs, which covered staff and capital costs. The capital costs associated with the apps related to app development and maintenance. The stand-alone app took approximately one month to develop, or 120 hours. The integrated app took approximately two months to develop, or 240 hours. It takes approximately two hours per week to maintain these apps. The apps were depreciated on a straight-line basis to reflect annual costs, in line with HIQA guidelines9. The unit cost of the equipment was calculated on a per-usage basis. We used data from CUMH to estimate the expected capacity use over a six-week period. This translates to 260 deliveries, giving an expected capacity use of 260 women to utilise these apps during the study time frame. The expected unit cost of the stand-alone app was €1.21 per woman and €2.32 for the integrated app (Table 1). Other costs, such as cost savings arising from a reduction of SSI following effective surveillance, were omitted given the objectives of this study.
We compared the costs and benefits of the proposed interventions within an informal cost-benefit analysis (CBA). The time horizon was six weeks, allowing for an estimation of the costs and benefits arising during the at-risk period of SSI. A net benefit analysis was estimated to compare costs and benefits;
where an activity was considered cost-beneficial if the difference was positive. To reflect the existence and extent of uncertainty in the input parameters, probabilistic sensitivity analysis (PSA) was performed10 using Microsoft Excel software11.
Results
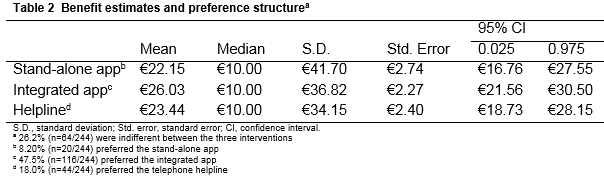
Women’s willingness-to-pay
Questionnaires were returned from 348 respondents, yielding a response rate of 91.8 per cent (sample characteristics can be made available by the authors on request). There is no significant difference between women’s WTP for the three interventions (Table 2). Women are willing to pay €22.15 (95% CI €16.76-27.55), €26.03 (95% CI €21.56-30.50), and €23.44 (95% CI €18.73-28.16) for the stand-alone app, integrated app, and helpline, respectively.
Women’s preference structure
Using available information on women’s WTP, as determined by the maximum WTP for a specific intervention, it is possible to identify women’s preference structure for the three interventions. Where clear preferences are observed, we find that approximately one in two women prefer the integrated app (47.5%; n=116/244), while the helpline is preferred by approximately one in five women (18.0%; n=44/244), which is more than double the number of women that prefer the stand-alone app (8.2%; n=20/244). One in four women (26.2%; n=64/244) are indifferent between the three interventions.
Cost estimates
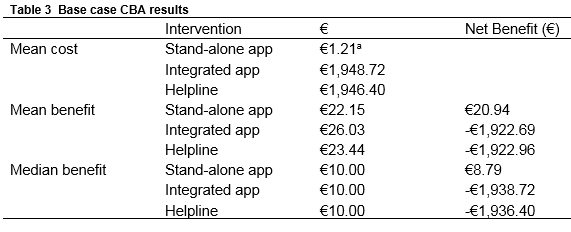
The estimated total service cost was €1.21 for the stand-alone app, €1,948.72 for the integrated app, and €1,946.40 for the helpline (Table 3). An additional cost associated with the integrated app related to the cost of employing a midwife to review data daily. To review data, one midwife is employed for five days per week, working two hours per day. At a unit cost of €32.44 per hour, the total staff cost was estimated at €1,946.40. A similar staff cost was obtained for the telephone helpline.
Cost-benefit findings
The net benefit results suggest that the stand-alone app is cost-beneficial. A positive net benefit (€20.94) is produced as women’s WTP for this service (€22.15) exceeds the cost (€1.21). When the median valuation is assumed, the results remain unchanged. In contrast, the integrated app and telephone helpline are not cost-beneficial as the cost of these services far exceed women’s WTP for them. (Similar results are obtained by the PSA, which can be made available by the authors on request).
Discussion
The aim of this research was not to provide conclusive evidence on the costs and benefits of the proposed interventions, but to learn about ways in which this research could be improved to more accurately examine the effectiveness and cost-effectiveness of these services. Many lessons are learned in this regard. While the CVM approach is regarded as a valid technique in eliciting benefit valuations, when applied to this area it likely produces results that are inconsistent with the expected benefits of the proposed interventions. Women valued the integrated app at €26.03, which is considerably smaller than the expected benefit of this service. We suspect there are two reasons for this under-valuation. First, the CVM scenario described the functionality of the app and how it could be used to communicate with a midwife, for example. It did not describe the potential benefits associated with early detection and treatment, which would likely influence women’s valuation of the app. If the app reduced the probability of developing a severe SSI relative to the stand-alone app or eliminated the likelihood of requiring further surgical intervention, then women may be willing to pay considerably more for this service. However, information on the effectiveness of the app in achieving these outcomes is required and can only be determined within a RCT. Second, it is likely women’s valuation of the integrated app and stand-alone app was considerably smaller than anticipated given women’s familiarity with paying small amounts for mobile apps. Consequently, the CVM approach is poorly equipped to capture meaningful benefit valuations here. An alternative approach which captures quality and length of life may be provided by utility weights, or the EQ-5D, which could be captured in a RCT.
In terms of costing the proposed interventions, the results do not represent the true cost of providing these services. We examined the direct service costs associated with providing the interventions, which included staff costs and app development and maintenance costs. Information on costs associated with repeat consultations with a GP or maternity hospital is important in determining the true cost, but could not be captured in this analysis given the lack of detailed patient level data.
It is difficult to say exactly what benefits could be achieved through the technology’s use, as it has yet to be field-tested. However, several important findings are obtained in this analysis. The aim of the mobile app was to examine the role technology can play in the delivery of health care and investigate whether advancements in technology can improve health, while reducing health care costs. The proposed integrated app is considerably expensive from a service perspective because it requires a midwife to review data daily. Further advancements in technology are required to eliminate these staff inputs. In the US, a similar mobile app is being developed to monitor and detect cases of diabetic retinopathy in patients with diabetes12. The functionality of the app is similar to the app presented here, in that patients record information and take photographs of their eye and upload these to the app. However, rather than employing a nurse or clinician to review these data, the researchers are developing an algorithm which evaluates the information and scans the photographs to detect cases of diabetic retinopathy12. To date, the researchers have found the algorithm accurately diagnoses cases of diabetic retinopathy 80% of the time, which is the same level of accuracy observed in clinicians12. To eliminate staff costs associated with the integrated app, a similar algorithm with comparable accuracy is required. This advancement in technology would transform the delivery of health care and achieve considerable reductions in health care costs. We are currently undertaking experimental work to develop a similar algorithm, which we aim to evaluate within a complete RCT.
Finally, women’s preferences for the three interventions followed a clear hierarchy. Almost one in two women (47.5%) preferred the integrated app over the alternative methods of surveillance. Given the increasing rate of CS in Ireland and decreasing rates of postpartum stay in hospital, the increased risk of SSI presents a considerable public health problem that requires a policy response. It seems women would prefer the integrated app to monitor surgical wound post-CS. Configuring health care services in this way would remove some of the inequalities that arise when health care is organised by government or professional bodies, however, the effectiveness and cost-effectiveness of this service needs to be considered.
Correspondence to:
Dr. Christopher G. Fawsitt, Senior Research Associate, Bristol Medical School, University of Bristol, Canynge Hall, 39 Whatley Road, Bristol, BS8 2PS, United Kingdom.
E-mail: [email protected]
Acknowledgements: We thank the participants of the study for taking the time to share their preferences with us. We also thank the team of contributors involved in the development of the mobile app: Dr Sabin Tabirca, Chris McCarthy, Lauren Violette and Dr. Laura Corkery.
Declaration of conflict of interest
All authors have nothing to declare.
Details of ethical approval: This study was granted ethical approval from Clinical Research Ethics Committee of the Cork Teaching Hospitals and the Division of Obstetrics and Gynaecology, Cork University Maternity Hospital.
Funding: This research was supported by the Strategic Research Fund, University College Cork.
References
1 HPSC. Point Prevalence Survey of Hospital Acquired Infection and Antimicrobial use in European Acute Care Hospitals: Dublin2012.
2 HSE. Caesarean Scetion Surgical Site Infection Surveillance: Wexford General Hospital2012.
3 NPRS. Perinatal Statistics Report 2012: Dublin2013.
4 NPRS. Perinatal Statistics Report 2014: Dublin2016.
5 Corcoran, S.; Jackson, V.; Coulter-Smith, S.; Loughrey, J.; McKenna, P.; Cafferkey, M. Surgical site infection after cesarean section: implementing 3 changes to improve the quality of patient care. American journal of infection control 2013, 41, 1258-1263.
6 StataCorps. Stata Statistical Software: Release 12: College Station: TX2012.
7 Frew, E. J.: Benefit assessment for cost-benefit analysis studies in health care: a guide to carrying out a stated preference willingness to pay survey in health care. In Applied Methods of Cost-Benefit Analysis in Health Care; McIntosh, E., Clarke, P. M., Frew, E. J., Louviere, J., Eds.; Oxfor University Press: New York, 2010.
8 Brouwer, W.; Rutten, F.; Koopmanschap: Costing in economic evaluations. In Economic Evaluation in Health Care: Merging Theory with Practice; Drummond, M., McGuire, A., Eds.; Oxford University Press: Oxford, 2001.
9 HIQA. Guidelines for the Economic Evaluation of Health Technologies in Ireland: Dublin2014.
10 Briggs, A.; Claxton, K.; Sculpher, M. J.: Decision Modelling for Health Economic Evaluation; Oxford University Press: Oxford, 2006.
11 Microsoft: Microsoft Excel. Microsoft Corporation: Redmond, WA, 2010.
12 Economist. Artificial intelligence in medicine: Now there’s an app for that. The Economist, September 19th, 2015.
(P635)