The Doctor Can See You Now: A Key Stakeholder Study Into The Acceptability Of Ambulance Based Telemedicine.
P Gilligan1, A Bennett2, A Houlihan2, A Padki, N Owens2, D Morris3, I Chochliouros3, A Mohammed, A Mutawa2, M A Eswararaj2, S Gannon2, A Alrmawi2, J Z Gasem2, P P N Sheung2, CTynan2, R Little2, W Merriman4, A Amadi-Obi1,2, L Kenna4, D A Alim2, C O’Donnel4.
1Department of Emergency Medicine, Beaumont Hospital, Beaumont Road, Dublin 9, Ireland
2Royal College of Surgeons in Ireland (RCSI), Dublin 2, Ireland
3LiveCity Project Team Members
4HSE Ambulance Service
Abstract
Using telecommunications technology it would be possible to link a patient and paramedic to a Doctor in the Emergency Department (ED) at the point of first patient contact. A questionnaire-based study on telemedicine in the pre-hospital environment involving patients, paramedics, doctors and nurses in the ED, was performed to assess if they would want and accept telemedicine in pre-hospital emergency care. When asked 98.5% (55) of patients, 89% (11) of doctors, 76% (14) of nurses and 91% (42) of ambulance personnel saw the potential of an audio-visual link from the pre-hospital environment to the ED. The potential benefits were felt to be in diagnosis of time-dependent illnesses, time management, increased hospital preparedness for incoming patients and increased triage efficiency. Stakeholder enthusiasm for pre-hospital telemedicine must be met with the technological requirements to provide such a service. As noted by one patient a pre-hospital audio-visual link to the ED could be “potentially a life saving service”.
Introduction
In a world where people can use smart phone technology to video link themselves to others in place of traditional phone calls it seems logical that a video link from the scene of an emergency to the ED could be useful. Telemedicine may be defined as the use of telecommunications to facilitate medical care. In recent years the ‘LiveCity Project’, funded by the European Commission,1 included the development of the hardware and software and the provision of a telecommunication infrastructure with high-speed Internet to allow for an encrypted audio-visual video communication from the site of an emergency to the ED of the research hospital. The concept was a hands free head mounted camera linked via a computer to the phone network to be used by the ambulance personnel to link patients with specific conditions to a Doctor in the receiving ED. Head mounting of the camera and microphone meant the Doctor in the ED could see what the ambulance personnel were seeing. This study was performed to see how the key stakeholders involved in emergency care: patients, ambulance personnel, doctors and nurses, would feel about a duplex (two way) audio and simplex (one way) video link from the scene of the emergency to the ED. This study also examined if these groups would want and accept telemedicine in pre-hospital emergency care and if they felt it could be potentially beneficial.
Methods
The study was performed in the ED of an 800 bed academic teaching hospital based in Dublin, Ireland. This adult only ED provides care to 50,000 patient attendances annually. Separate questionnaires were developed for patients and staff. The questionnaires for the medical and nursing staff ascertained a) demographic details, b) comfort levels with technology and c) willingness to use telemedicine in different circumstances (stroke/myocardial infarction - MI /trauma). The questionnaire for ambulance personnel analysed a) demographic details and b) attitudes and perceptions of the use of video conferencing in pre-hospital care. The patient questionnaire analysed a) demographic details, b) ambulance service use and emergency department attendance and c) comfort with technology and their attitudes towards the use of telemedicine by ambulance personnel.
The questionnaire results provided both qualitative and quantitative data, which were analysed separately. Statistical analysis was performed using SPSS software. The comments and statements from the qualitative data were analysed using simple thematic analysis. Ethical approval was obtained from the Research and Ethics Committee of the teaching hospital in which the study was performed.
Results
ED Staff Demographics
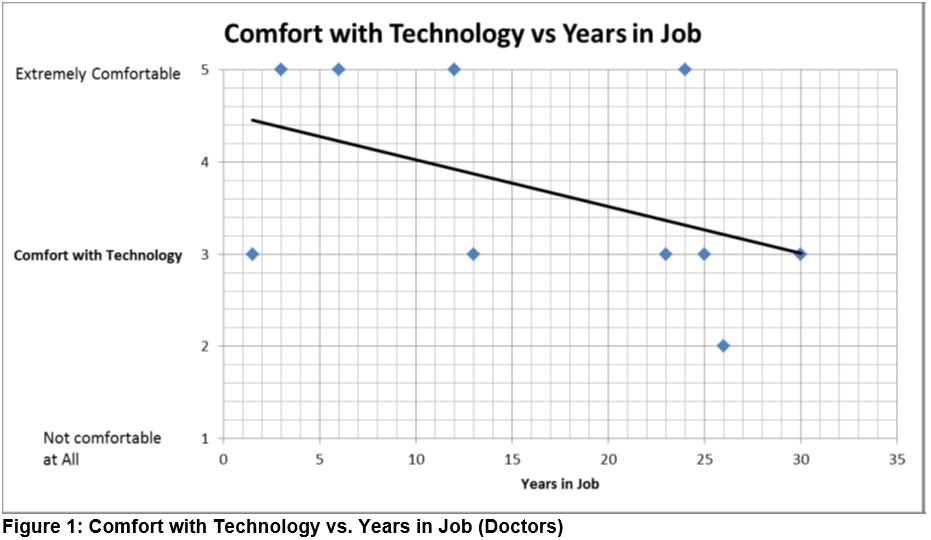
The results of the staff questionnaire showed that of the 31 doctors and nurses questioned, 38.7% (12) were doctors. There was an even split of 50% male and female doctors, whilst 77.7% (15) of the nurses (19) were female. Of the 29 hospital staff who gave their age 18 (62%) were under 40 years of age. The more experienced staff members tended to describe themselves as less comfortable with the use of technology. Figure 1 depicts the Doctors’ comfort with technology against their years working.
 Outcome
Outcome
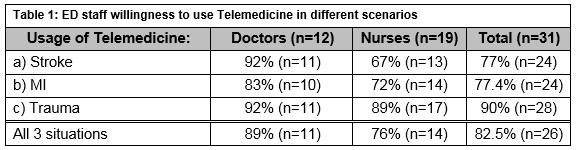
The attitudes regarding the use and implementation of telemedicine in the pre-hospital environment were very positive, as illustrated in Table 1.
When asked what potential benefits there would be from the use of video communication technology, 41.4% (n=13) of ED staff answered that it would make the ED more efficient with regards to the diagnosis of time-dependent illnesses, improve time management in the ED, increase hospital preparedness for incoming patients and increase timeliness of triage.
When asked about any concerns or apprehensions about the video-link technology, both doctors (12) and nurses (19) were most concerned about:
a) Patient confidentiality 64.5% (n=20)
b) Technological limitations 45.2% (n=14)
c) Staff liability 16.1% (n=5)
Ambulance Personnel Demographics
Fifty ambulance personnel who brought patients to the ED were surveyed of whom 46 (92%) responded. These were drawn from 3 ambulance services and included; 32 Dublin Fire Brigade (DFB) personnel, 12 Health Services Executive (HSE) personnel and 2 Airport Fire Service (APFS) personnel. Their clinical grades are shown in Figure 2.
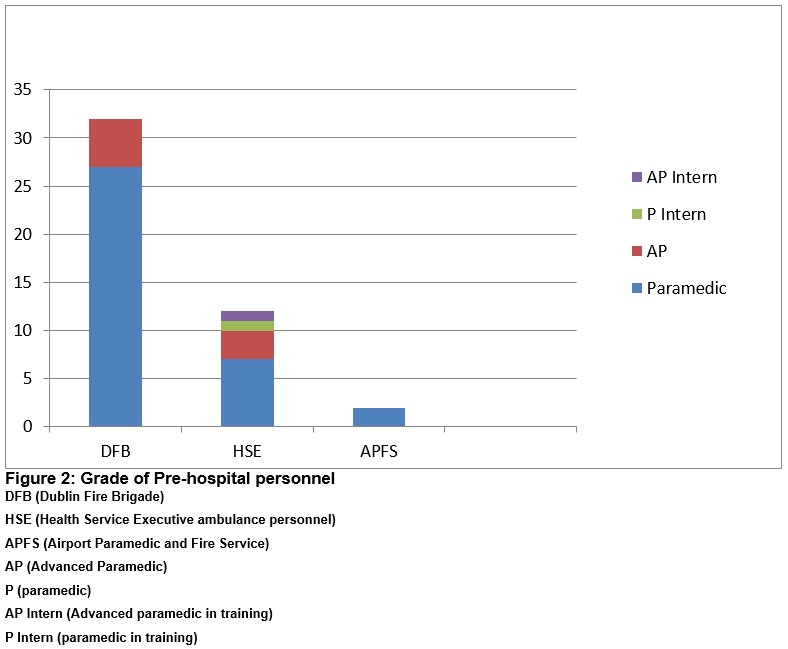
Males accounted for 87% (40). The mean age was 38.2 years (range 27-62 years) and the mean pre-hospital experience was 11 years (range 1-40 years)
Outcome
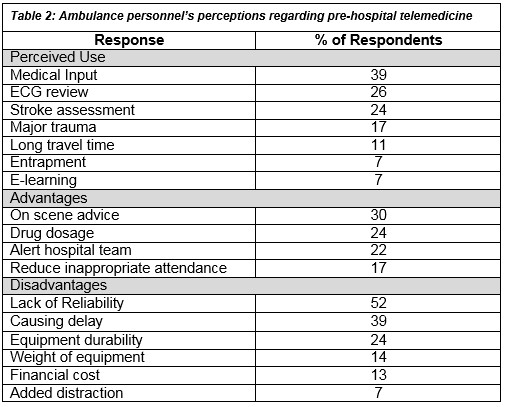
The majority of ambulance personnel respondents i.e. 91% (41) saw a positive role for video communication technology in pre-hospital care and 67% (31) would be willing to adopt it in their own practice. Table 2 shows the suggested uses and possible advantages and disadvantages of telemedicine in the pre-hospital environment according to the ambulance personnel.
Patient Demographics
Fifty-six patients completed the questionnaire study. Males accounted for 69.6% (n=39). The age of patient respondents ranged from 21 to 89 years of age. Forty-six patients (82.1%) had used the ambulance service in the past between 0 to 5 times, 14.3% (8) had used the service 6 to 10 times and 3.6% (2) had used it more than 20 times.
When asked to rate their comfort with new technologies such as computers, tablets and smartphones on an adjectival scale rating from “extremely comfortable” to “not at all comfortable” 20 patients (35.7%) said they were extremely comfortable, 23.2% (13) were very comfortable with technology, 19.6% (11) were moderately comfortable and 8 (14.3%) patients described themselves as not at all comfortable with these technologies.
Fifty-five (98.5%) patients said they would like the ambulance service to use video link telemedicine technology to contact a doctor in the ED so they could be assessed before arriving at hospital. In relation to the use of this technology in possible stroke cases examples of the responses given were: “It could make the difference as to whether I live or die, so I’m definitely in favour.’’ “Potentially a lifesaving service’’ and “Time saves lives.’’ In relation to the use of this technology in a major trauma case, responses given included: “It could be important to determine which hospital they need to go to” and “if they are aware of the type of treatment required before arriving at hospital, it will reduce wait time”. In cases of possible MI and the use of this technology, responses given included; “Time is critical here so could be lifesaving” and “Certainly does no harm and could save a life”.
Discussion
Early intervention in medical emergencies improves clinical outcomes1,2,3,4. The advantage of an early pre-hospital diagnosis is supported by various literature, for example patient transfer directly to a cardiac catheter laboratory for percutaneous coronary intervention after pre-hospital diagnosis of ST elevation myocardial infarction (STEMI) in a telemedicine equipped ambulance has been shown to reduce treatment delay5,6,7,8.9 and reduce mortality from myocardial infarction10. Telemedicine in MI has shown a positive impact5 and in stroke management telemedicine is now recommended by the American Heart Association to reduce treatment delays11, yet the adoption of these emerging technologies has been slow.12 End user engagement in the adoption of new technologies in healthcare does not depend solely on clinical validation and regulatory considerations13. With this in mind we sought to establish patients’, ambulance personnel’s and hospital staff’s willingness to accept telemedicine in the pre-hospital environment. Eighty nine percent (n=10) of doctors, 76%(n=14) of nurses and 91% (n=41) of ambulance personnel saw the potential for telemedicine in pre-hospital care and our results indicate that they thought it would be most useful in dealing with situations where early diagnosis and intervention were key to patient recovery.
The vast majority (98.5%) (n=55) of the patient group had very positive attitudes towards the use of the video link technology by the ambulance service. This finding is in keeping with a number of international studies assessing patient’s attitudes towards and willingness to use telemedicine3,4. The patients’ responses noted the critical importance of time in assessing and treating a MI and stroke, and the potential for this technology to be lifesaving by reducing the time scale involved. This finding is supported by other studies showing that Telemedicine is feasible and effective in decreasing treatment times and is associated with a high diagnostic accuracy rate, there is higher rates of positive task completion than in regular ambulances, and it has demonstrated that telemedicine based stroke evaluation is completed with comparable accuracy to the standard way of delivering care14.
It is important to note that the doctors and nurses surveyed raised very valid concerns surrounding patient confidentiality, hardware and software issues with the technology, network issues and operative responsibility and governance of this new technology and the associated liability. Doctors and nurses expressed concerns that because the patient video data is to be transferred over a wireless network to a screen in the Emergency Department, there could be the potential for a breach in patient confidentiality. With regards to technological limitations, staff members were concerned that there may be difficulty operating the technology in certain situations such as adverse weather conditions, low light levels and in remote areas without network coverage. Concerns were also expressed regarding the quality of the video and the limitation of the view. The third overall concern was one of liability. Doctors had concerns about the apportioning of blame in the event of an incorrect diagnosis made over a telemedicine link.
These concerns are supported by other research such as a study investigating the feasibility of telemedicine in pre-hospital stroke management, which found that in 18 of 30 scenarios, National Institutes of Health Stroke Scale assessment could not be performed due to absence or loss of audio-video signal15. However if such technical issues can be addressed and managed adequately, telemedicine has been found to be efficient and reliable in various emergency situations, such as in the remote assessment of stroke severity in fast-moving ambulances using a system dedicated to pre-hospital telemedicine and 4G technology16.
Ireland currently has as part of the ‘National Clinical Programmes’ a National Acute Coronary Syndrome pathway that involves the direct transfer of patients with ST elevation Myocardial Infarction (STEMI) to a unit offering percutaneous coronary intervention(PCI). The ambulance service will telephone the PCI centre and forward an ECG by fax or smart phone image to the centre who will then decide on the basis of ECG findings and history whether or not to accept the direct transfer of the patient to the coronary catheterization laboratory17.
In Ireland, paramedics receive training in recognizing patients who may be having a stroke with features of facial droop, arm weakness, slurred speech and recent onset of such symptoms (a F.A.S.T. assessment). Patients who are found to have features suggestive of a stroke may have their details telephoned through to the receiving hospital that can then have a stroke team ready to assess such patients on their arrival to the Emergency Department. Stroke specialists in some hospitals in Ireland are performing telemedical stroke assessments at a distance using technology brought to the patient’s bed side which allows the specialist to see and speak with the patient who may be suffering a stroke18.
Since August 2001 the Emergency Department in Cork University Hospital has provided a Tele-Medical Assistance Service (TMAS) to the Irish Coast Guard and advanced paramedics. The red phone in the Emergency Department can accept calls that may originate from VHF / MHF radio, GSM or Satellite sources and advice can be given by a senior decision maker in the Emergency Department to the rescue services19.
For those using the ambulance service the first point of contact with healthcare is the ambulance personnel. Currently if a paramedic requires further medical input they obtain it via a telephone link to a doctor. This current practice does not facilitate the ED doctor in visualizing the patient and ascertaining other potentially vital information directly from the patient. Telemedicine in the pre-hospital setting could bring a hospital based specialist opinion to the patient sooner. It also has the potential to open up faster and more efficient communication channels between the patient, ambulance personnel and the ED staff, through the immediate transmission of medical data, informatics and images from the ambulance setting to the ED.
The challenge now is to address the hardware, software and network requirements of providing a reliable, safe, real time audio-visual link from wherever the patient is to the Emergency Department because the majority of key stakeholders being ambulance personnel, patients, doctors and nurses feel a pre-hospital audio-visual link to the ED would help to improve outcomes and potentially save lives.
Correspondence: Dr Peadar Gilligan, Department of Emergency Medicine, Beaumont Hospital, Beaumont Road, Dublin 9, Ireland
Email: [email protected]
Conflict of interest
There is no conflict of interest for the authors involved in this study.
Acknowledgements
The RCSI research Department and the European Commission for funding the research.
References
1. Europe's Information Society. Live City: Live Video-to-Video Supporting InteractiveCity Infrastructure [Video on the internet] [Cited 21 May 2013]. Available from: http://ec.europa.eu/information_society/apps/projects/factsheet/index.cfm?project_ref=297291.
2. Whan P, Brown NA, Wootton R. A Bibliographic Snapshot of the Telemedicine Citation Literature. J Telemed and Telecare. 2006;12(7):95–102.
3. Meher SK, Tyagi RS, Chaudhry T. Awareness and attitudes to telemedicine among doctors and patients in India. J Telemed Telecare. 2009;15(3):139-41.
4. Terschüren C, Mensing M, Mekel OC. Is telemonitoring an option against shortage of physicians in rural regions? Attitude towards telemedical devices in the North Rhine-Westphalian health survey, Germany. BMC Health Serv Res. 2012;12-95.
5. Afolabi BA, Novaro GM, Pinski SL, Fromkin KR, Bush HS. Use of the prehospital ECG improves door-to-balloon times in ST segment elevation myocardial infarction irrespective of time of day or day of week. Emerg Med J. 2007;24(8):588-91.
6. Brunetti ND, De Gennaro L, Amodio G, Dellegrottaglie G, Pellegrino PL, Di Biase M, Antonelli G. Telecardiology improves quality of diagnosis and reduces delay to treatment in elderly patients with acute myocardial infarction and atypical presentation. Eur J Cardiovasc Prev Rehabil. 2010;17(6):615-20.
7. Sejersten M, Sillesen M, Hansen PR, Nielsen SL, Nielsen H, Trautner S, Hampton D, Wagner GS, Clemmensen P. Effect on treatment delay of prehospital teletransmission of 12-lead electrocardiogram to a cardiologist for immediate triage and direct referral of patients with ST-segment elevation acute myocardial infarction to primary percutaneous coronary intervention. Am J Cardiol. 2008;101(7):941-6.
8. Terkelsen CJ, Lassen JF, Nørgaard BL, Gerdes JC, Poulsen SH, Bendix K, Ankersen JP, Gøtzsche LB, Rømer FK, Nielsen TT, Andersen HR. Reduction of treatment delay in patients with ST-elevation myocardial infarction: impact of pre-hospital diagnosis and direct referral to primary percutanous coronary intervention. Eur Heart J. 2005;26(8):770-7.
9. Zanini R, Aroldi M, Bonatti S, Buffoli F, Izzo A, Lettieri C, Romano M, Tomasi L, Ferrari MR. Impact of prehospital diagnosis in the management of ST elevation myocardial infarction in the era of primary percutaneous coronary intervention: reduction of treatment delay and mortality. J Cardiovasc Med (Hagerstown). 2008;9(6):570-5.
10. Sanchez-Ross M, Oghlakian G, Maher J, Patel B, Mazza V, Hom D, Dhruva V, Langley D, Palmaro J, Ahmed S, Kaluski E, Klapholz M. The STAT-MI (ST-Segment Analysis Using Wireless Technology in Acute Myocardial Infarction) trial improves outcomes. JACC Cardiovasc Interv. 2011;4(2):222-7.
11. Schwamm LH, Audebert HJ, Amarenco P, Chumbler NR, Frankel MR, George MG, Gorelick PB, Horton KB, Kaste M, Lackland DT, Levine SR, Meyer BC, Meyers PM, Patterson V, Stranne SK, White CJ; American Heart Association Stroke Council; Council on Epidemiology and Prevention; Interdisciplinary Council on Peripheral Vascular Disease; Council on Cardiovascular Radiology and Intervention. Recommendations for the implementation of telemedicine within stroke systems of care: a policy statement from the American Heart Association.Stroke. 2009;40(7):2635-60.
12. Walker J, Whetton S. The diffusion of innovation: factors influencing the uptake of telehealth.J Telemed Telecare. 2002;8 S3:73-5.
13. Bernstein ML1, McCreless T, Côté MJ. Five constants of information technology adoption in healthcare. Hosp Top. 2007;85(1):17-25.
14. Rogers H, Madathil KC, Agnisarman S, Narasimha S, Ashok A, Nair A, Welch BM, McElligott JT. A Systematic Review of the Implementation Challenges of Telemedicine Systems in Ambulances. Telemed J E Health. 2017;23(9):707-717.
15. Liman TG1, Winter B, Waldschmidt C, Zerbe N, Hufnagl P, Audebert HJ, Endres M. Telestroke ambulances in prehospital stroke management: concept and pilot feasibility study. Stroke. 2012;43(8):2086-90
16. Van Hooff RJ, Cambron M, Van Dyck R, De Smedt A, Moens M, Espinoza AV, Van de Casseye R, Convents A, Hubloue I, De Keyser J, Brouns R. Prehospital unassisted assessment of stroke severity using telemedicine: a feasibility study. Stroke. 2013;44(10):2907-9.
17. National Clinical Programmes; Acute Coronary Syndrome.[Cited 20 Feb 2018]. Available from: https://www.hse.ie/eng/about/who/cspd/ncps/acs/
18. Stroke Clinical Care Programme Model of Care - HSE [Cited 20 Feb 2018]. Available from:https://www.hse.ie/eng/services/publications/clinical...and.../stroke-model- of- care.
19. Medico Cork Background Information.[Cited 20 Feb 2018].
Available from: http://emed.ie/Administration/Medico/Medico_history.php
(P769)
