The Prevalence of Severe Sepsis or Septic Shock in an Irish Emergency Department
C McNevin1, R McDowell2, F Fitzpatrick,3,4 R O’Sullivan,5,6 A Wakai7,8
1Medical School, Royal College of Surgeons in Ireland (RCSI), Dublin 2, Ireland.
2RCSI Department of General Practice, Division of Population Health Sciences (PHS), Dublin 2, Ireland.
3Department of Clinical Microbiology, RCSI Education & Research Centre, Beaumont Hospital, Dublin 9, Ireland.
4Department of Microbiology, Beaumont Hospital, Dublin 9, Ireland.
5School of Medicine, University College Cork, Cork
6Bon Secours Hospital, Cork.
7Department of Emergency Medicine, Beaumont Hospital, Dublin 9, Ireland.
8Emergency Care Research Unit (ECRU), RCSI Department of General Practice, 123 St Stephens Green, Dublin 2, Ireland.
Abstract
Severe sepsis and septic shock are among the leading causes of death globally. Despite the central role the emergency department (ED) plays in the early identification of patients presenting to hospital with sepsis, the prevalence of severe sepsis and septic shock in the Irish ED setting has not been described. The primary aim of this study was to measure the prevalence of severe sepsis or septic shock in an Irish adult ED setting. The clinical records of patients presenting to the ED over a four-week period were retrospectively reviewed to determine if they met the current Health Service Executive (HSE) criteria for severe sepsis or septic shock. Overall, 3,585 adult patients attended the ED during the study period, with 42 patients meeting the criteria for severe sepsis or septic shock. The ED prevalence of severe sepsis or septic shock was 11.7 patients (95% CI 8.1 – 15.4%) per 1000 ED attendances.
Introduction
In Ireland, up to 60% of all hospital deaths have a sepsis or infection diagnosis1. Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection2. It encompasses a clinical spectrum of, increasingly severe systemic inflammatory responses to infection including “uncomplicated” sepsis, severe sepsis and septic shock. Severe sepsis and septic shock are among the leading causes of death globally, accounting for more than 15 million deaths worldwide annually3. Severe sepsis and septic shock remain a major cause of emergency department (ED) attendances and intensive care unit (ICU) admissions and are associated with significant morbidity, mortality and healthcare costs4,5. In-hospital mortality for severe sepsis and septic shock can approach 50% to 60% once shock is present, consequently the public health burden of these conditions is substantial4, 6, 7.
We recently reported, for the first time, the prevalence of “uncomplicated” sepsis in an Irish ED8. Although the epidemiology of severe sepsis and septic shock in the ED setting has been reported in other countries4, 9-11, it has not previously been reported in Ireland. The primary aim of this study was to measure the ED prevalence of severe sepsis or septic shock in adult patients in an Irish ED. The secondary aim was to determine the demographic and clinical characteristics of ED patients who met the criteria for severe sepsis or septic shock.
Methods
This study was performed in the ED of Beaumont Hospital, Dublin. The annual census of the ED is approximately 50,000 patients. The Beaumont Hospital Ethics (Medical Research) Committee approved the study. This study used a cross-sectional secondary data analysis design. Data from a cross-sectional study conducted to determine the proportion of patients who met the criteria for “uncomplicated” sepsis was analysed to identify the subset of patients who met the criteria for severe sepsis or septic shock8. The cross-sectional study involved screening the clinical records of consecutive patients presenting to the ED over a one-month study period (July-August 2015) for sepsis using the Health Service Executive (HSE) Sepsis Screening Form12. The definitions of severe sepsis and septic shock employed in this study were those used in the HSE Sepsis Screening Form12
Data on patient age, gender, temperature, heart rate, systolic blood pressure (SBP), mean arterial pressure (MAP), respiratory rate, need for oxygen to achieve a saturation > 90%, Glasgow Coma Scale (GCS) score, blood glucose, white cell count, presence or absence of diabetes, blood lactate, urine output, serum creatinine, serum bilirubin, prothrombin time (PTR), activated partial thromboplastin time (aPTT) and platelet count were obtained from the clinical records. Where one or more of the systemic inflammatory response syndrome (SIRS) criteria used to diagnose sepsis had not been recorded for an individual, the diagnostic criteria were applied to all available data.
Data was analysed with descriptive statistics and reported as frequencies, proportions, percentages, medians and interquartile ranges (IQR). Point estimates (p-values) and interval estimates (95% confidence intervals [CIs]) for the proportion of patients who met the criteria for severe sepsis or septic shock and the prevalence of severe sepsis or septic shock were calculated. The Mann-Whitney U test was used to examine whether there was a significant difference in the underlying age distributions of ED patients with and without severe sepsis or septic shock, and whether there was a significant difference in the age distributions of the male and female patients who met the criteria for severe sepsis or septic shock. The chi-squared test was used to examine whether gender and sepsis status were independent. A p-value of less than 0.05 was considered statistically significant. Analyses were performed using Microsoft Excel and Statistical Package for the Social Sciences (SPSS) version 21.0 (IBM, 2012).
Results
Patients who met the criteria for severe sepsis or septic shock
Overall, 42 of 3585 ED patients met the criteria for severe sepsis or septic shock. This represents 11.7 patients with severe sepsis or septic shock per 1000 ED attendances or 1.17% (95% CI 0.81 – 1.54 %) . Table 1 shows the number of SIRS criteria met by ED patients who met the criteria for severe sepsis or septic shock. There was a significant difference in the age distributions of ED patients with severe sepsis or septic shock and those without (p < 0.001; Table 2); patients who met the criteria for severe sepsis or septic shock were on average older than those who did not. There was no significant difference in the gender distributions of ED patients with and without severe sepsis or septic shock (p = 0.25); 59.5% of patients with severe sepsis or septic shock were female whereas 50.6% of patients without sepsis were female (Table 2). There was a statistically significant difference between the underlying age distributions of the male and female patients who met the criteria for severe sepsis or septic shock (p=0.03). Among patients who met the criteria for severe sepsis or septic shock, males (median age 75 years, IQR 68.5 – 82 years) were significantly older than females (median age 68 years, IQR 53.5 – 78 years).
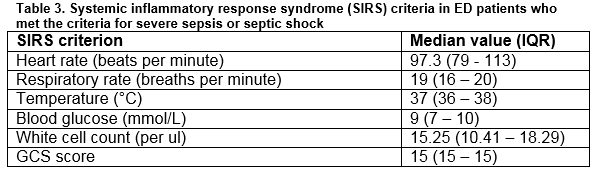
Regarding the SIRS criteria in the patients who met the criteria for severe sepsis or septic shock, the median heart rate was 97.3 beats per minute (IQR = 79 - 113 beats per minute), the median respiratory rate was 19 breaths per minute (IQR = 16-20 breaths per minute) and the median temperature was 37°C (IQR = 36 - 38°C). Nine patients (21.4%) who met the criteria for severe sepsis or septic shock had an altered mental status, and the median GCS score was 15. The median blood glucose was 7.0 mmol/L (IQR = 6 - 9 mmol/L) and the median white cell count was 15.25 x 109/μl (IQR = 10.41 – 18.29 x 109/μl) (Table 3).
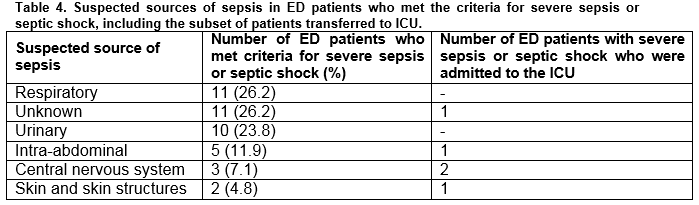
The most common suspected source of sepsis in patients who met the criteria for severe sepsis or septic shock was the respiratory system (n=11, 26.2%). The genitourinary system was the second most common source of sepsis (n=10, 23.6%) (Table 4). There were as many patients with an unknown source of sepsis as those with a suspected respiratory source (n=11, 26.2%).
Patients transferred to the intensive care unit (ICU)
Five patients with severe sepsis or septic shock were transferred to the ICU for further management. These patients had a median age of 61 (IQR = 49 - 76 years, range 39-77 years). The suspected sources of sepsis in these patients are outlined in Table 4.
Discussion
The epidemiology of severe sepsis or septic shock in the Irish ED setting is currently unknown. The primary aim of this study was to measure the prevalence of severe sepsis or septic shock in an Irish adult ED setting. We found that the prevalence is 11.7 sepsis patients per 1,000 ED attendances. Our study of 3,585 patients is more than twice the number of patients required (1,546) to estimate the prevalence of severe sepsis or septic shock in the ED with 95% confidence, allowing for a one percent margin of error and assuming that the prevalence of severe sepsis or septic shock in the ED is 5% (the upper limit of the 95% confidence interval of the estimated proportion of patients with “uncomplicated sepsis” in this sample)8.
Prevalence data are critical in determining healthcare resource allocation. Due to the fact that the majority of patients with severe sepsis are admitted to ICUs from the ED13, measuring the ED prevalence of severe sepsis and septic shock is important in determining healthcare resource allocation, such as critical care utilisation and ICU admissions. The epidemiology of severe sepsis and septic shock in the ED setting has been reported in the United States of America4,9-11, and Brazil14. Wang (2007) reported that of 331.5 million adult ED visits in the United States over four years, approximately 2.3 million visits (571,000 annually, 0.69%; 95% CI, 0.61-0.77%) were for suspected severe sepsis. In a single centre prospective study over a six-month period, Rezende reported a prevalence of 64.1 (342 / 5332) per 1000 (95% CI, 57.5 – 70.8) of severe sepsis/septic shock in Brazilian ED patients14.
In the UK, Cowan performed a four week single-centre retrospective observational study and reported an ED prevalence of severe sepsis of 21.6 per 1000 (95% CI, 14.5 – 28.6)9. However, in terms of study methodology, only one of these reports, a UK study10 is directly comparable to our study. They aimed to measure the incidence of ED patients with SIRS, “uncomplicated” sepsis, severe sepsis and septic shock and found that the incidence of patients with severe sepsis or septic shock is 8.6 (95% CI, 6.1 – 11.0) per 1000 patients attending the ED10. Similar to our initial objective at the outset of this study, they intended to separately categorise severe sepsis and septic shock; however, this requires data on whether hypotension persisted despite adequate fluid resuscitation which were not reliably and consistently available in the patient records, so they analysed the severe sepsis and septic shock groups as a single group (“severe sepsis or septic shock”). This is comparable to our estimate of severe sepsis and septic shock being 11.7 (95% CI 8.1 – 15.4%) per 1000 ED attendances.
Our study found that there was a significant difference in the age distribution of ED patients with severe sepsis or septic shock and those without severe sepsis or septic shock. Patients who met the criteria for severe sepsis or septic shock were significantly older than those without severe sepsis or septic shock. This is consistent with previous studies reporting sepsis as a disease of the elderly 4,5,10,11,14. This is explained in part by the presence of comorbid conditions, biological immunosenescence, altered cytokine production and coagulation abnormalities15.
The design of this study has limitations that have previously been described8. The prevalence estimated in this study could be an underestimate on the basis that organ dysfunction is not always documented in the ED as all relevant laboratory results may not be available. Notwithstanding these limitations, this study found that the ED prevalence of severe sepsis or septic shock was 11.7 (95% CI 8.1 – 15.4%) per 1000 ED attendances per 1000 ED attendances. This translates to approximately one in every 100 patients attending the ED meeting the criteria for severe sepsis or septic shock.
Conflict of Interest
The authors have read and understood IMJ policy on declaration of interests and declare that they have no competing interests.
Correspondence
Dr. Abel Wakai, Emergency Care Research Unit, Department of General Practice, Royal College of Surgeons in Ireland, 123 St. Stephen's Green, Dublin 2
Email: [email protected]
Phone: +353 1 402 2304/06
Acknowledgements
The data presented here are as a result of a valuable collaborative process between the ED administrative, nursing, IT and medical staff in Beaumont Hospital. We thank them for their help and contribution.
References
1. The National Clinical Effectiveness Committee (NCEC). Sepsis Management. National Clinical Guideline. 2014.
2. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). Jama. 2016;315(8):801-10.
3. Adhikari NK, Fowler RA, Bhagwanjee S, Rubenfeld GD. Critical care and the global burden of critical illness in adults. Lancet. 2010;376(9749):1339-46.
4. Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Critical care medicine. 2001;29(7):1303-10.
5. Wang HE, Shapiro NI, Angus DC, Yealy DM. National estimates of severe sepsis in United States emergency departments. Critical care medicine. 2007;35(8):1928-36.
6. Dombrovskiy VY, Martin AA, Sunderram J, Paz HL. Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003. Critical care medicine. 2007;35(5):1244-50.
7. Gaieski DF, Edwards JM, Kallan MJ, Carr BG. Benchmarking the Incidence and Mortality of Severe Sepsis in the United States*. Critical care medicine. 2013;41(5):1167-74.
8. McNevin C, McDowell, R, Fitzpatrick F, Gilligan P, Wakai, A. What Proportion of Patients Meet the Criteria for Uncomplicated Sepsis in an Irish Emergency Dept? . Irish medical journal. 2016;109(7).
9. Cowan SL, Holland JA, Kane AD, Frost I, Boyle AA. The burden of sepsis in the Emergency Department: an observational snapshot. European journal of emergency medicine : official journal of the European Society for Emergency Medicine. 2015;22(5):363-5.
10. Majuran M, Clancy M. Determination of the size of the different sepsis categories presenting to a UK teaching hospital emergency department. Emergency medicine journal : EMJ. 2008;25(1):11-4.
11. Gray A, Ward K, Lees F, Dewar C, Dickie S, McGuffie C. The epidemiology of adults with severe sepsis and septic shock in Scottish emergency departments. Emergency medicine journal : EMJ. 2013;30(5):397-401.
12. Health Service Executive (HSE). Sepsis 2013 [Available from: http://www.hse.ie/eng/about/Who/clinical/natclinprog/sepsis/Emergency Department Adult Sepsis Pathway.pdf
13. McIntyre LA, Fergusson D, Cook DJ, Nair RC, Bell D, Dhingra V, Hutton B, Magder S, Hébert PC; Canadian Critical Care Trials Group. Resuscitating patients with early severe sepsis: a Canadian multicentre observational study. Canadian journal of anaesthesia = Journal canadien d'anesthesie. 2007;54(10):790-8.
14. Rezende E, Silva JM, Jr., Isola AM, Campos EV, Amendola CP, Almeida SL. Epidemiology of severe sepsis in the emergency department and difficulties in the initial assistance. Clinics (Sao Paulo, Brazil). 2008;63(4):457-64.
15. Starr ME, Saito H. Sepsis in old age: review of human and animal studies. Aging and disease. 2014;5(2):126-36.
(P692)