The Uptake of Human Papillomavirus Vaccine In Irish Schools: The Impact Of Disadvantage
C Migone1, T Barrett2, S Cotter3, A Clarke2, B Corcoran2
1. Department of Public Health, Health Service Executive-East, Dr Steevens’ Hospital, Dublin 8, Ireland
2. National Immunisation Office, Units 8-9 Manor Street Business Park, Manor Street, Dublin 7, Ireland
3. Health Protection Surveillance Centre, 25-27 Middle Gardiner Street, Dublin 1, Ireland
Abstract
HPV vaccine Gardasil© is offered to girls in first year of secondary school in Ireland. We aimed to determine the association between HPV vaccine uptake among girls for academic year 2013/2014, by school and school characteristics: socioeconomic disadvantage and religious ethos. The National Schools Immunisation System (SIS) was searched to determine HPV vaccine uptake in schools for 2013/2014 (prior to recent anti-HPV vaccine publicity). The disadvantaged status and ethos of each school was added to the report. In total 577 schools were identified. Mean vaccine uptake was 83.7%. Disadvantaged schools had a lower mean uptake (%) than other schools (79.4% vs 85.0%, difference 5.58%, 95%CI 2.69-8.21) and were twice as likely to have an uptake of ≤50% (OR 2.07, 95% CI 2.76 - 5.18). No difference was found between schools of different ethoses. HPV vaccine uptake is lower in disadvantaged Irish schools. Policies should be developed to ensure a more equitable uptake of HPV vaccine.
Introduction
Human Papillomavirus (HPV) vaccine was introduced into the national immunisation programme in 2010 to protect girls against HPV high-risk types that cause cervical cancer. Quadrivalent HPV vaccine Gardasil© is offered to all girls in first year of second level school as part of the National Schools Immunisation Programme. The vaccine protects against HPV types 16 and 18 which cause 70% of cervical cancers and protects against HPV types 6 and 11, responsible for 90% of genital warts1. It is given by school vaccination teams from 32 Local Health Offices around the country. The vaccine is not available through general practitioners except by private payment. In 2013/2014, three doses of HPV vaccine were recommended at 0, two and 6 month intervals. Cervical cancer is known to disproportionally affect women from socio-economically disadvantaged groups due to a combination of factors including risk factors and lower uptake of cervical screening. HPV vaccination programmes should therefore aim to protect all women, but particularly those from disadvantaged backgrounds. However, opportunistic uptake of HPV vaccine is known to be lower amongst girls from disadvantaged backgrounds1,2. School vaccination programmes have been shown to maximise uptake of vaccines3 since access to the cohort for vaccination is already established and should thus minimise differences in HPV vaccination uptake between socioeconomically disadvantaged populations and the general population2. However, there is evidence that disparities in uptake may still exist in school vaccination programmes4-7.
In Ireland, it is not known if uptake of HPV vaccine in schools is affected by disadvantage. Whether religious beliefs have an impact on uptake is also unknown, although this is not currently supported by evidence from other countries8,9. Limitations of existing health information systems and data protection legislation mean that it is not possible for public health authorities to access individual level data such as address, ethnic origin or socioeconomic status for students in the cohort for vaccination; however data are available of the characteristics of each school involved in the Schools Immunisation Programme.
The aims of our study were to determine the association between HPV vaccine uptake among the cohort of students eligible for vaccination for the academic year 2013/2014, by school and school characteristics i.e. socioeconomic deprivation, religious ethos and co-educational status in order to assess the need for additional targeted measures to improve uptake. Our study was undertaken before anti-HPV vaccine publicity negatively affected HPV vaccine uptake in schools and uptake rates refer to uptake at the time the study was conducted.
Methods
The Irish Schools Immunisation System (SIS) is a national web-based system that records uptake for school vaccines for each academic year. Prior to each academic year, the Department of Education and Skills (DES) provides the Schools Immunisation Programme with the number of girls in the cohort to be vaccinated in each secondary school. Once the vaccination programme for that year is completed, vaccination uptake for each school is entered into SIS in each region. Data is collected centrally by the National Immunisation Office, and sent to the Health Protection Surveillance Centre (HPSC) where it is further validated and national uptake statistics are produced10. A total of 864 schools were identified through the SIS system. Schools for students with intellectual or physical disabilities were excluded from analysis (n=141) as in these schools the immunisation programme is delivered by age rather than class cohort. Boys-only schools (n=107) were excluded. Schools reporting a cohort of 0 (i.e. no girls in the class) at the beginning of the academic year were also excluded (n=39). In total 577 schools were included.
A SIS report was generated of HPV vaccine uptake for each school, defined as the proportion of students who received 3 doses of vaccine for the 2013/2014 academic year (at the time three doses were recommended at 0, 2 and 6 month intervals). Schools that reported an uptake of >100% (n=8), because of intake of one or more pupils after the date of the school census, were assumed to have an uptake of 100%. School characteristics were determined through searching the DES website i.e. co-educational or girls-only, religious ethos and schools that have been designated as DEIS schools (delivering equality of opportunity in schools i.e. schools at educational and social disadvantage). Second-level schools are selected as DEIS schools by the Educational Research Centre on behalf of the DES. The DEIS status of each school is determined using centrally-held data from the Post-Primary Pupils and State Examinations Commission databases using the following parameters: medical card* data for Junior Certificate candidates in each school, Junior Certificate retention rates by school and Junior Certificate exam results aggregated to school level11.
For the purposes of this study, the characteristics of each school were added to the SIS report. Associations between variables were explored using the χ2-test for categorical variables and student t-test, Kruskal-Wallis, and Mann-Whitney U test for continuous variables. Statistical significance was set at p <0.05. Univariate analysis was performed initially to identify significant determinants of HPV vaccine uptake in schools of ≤50% in schools. Multivariate analysis was then performed, entering all determinants simultaneously. Data was analysed using IBM SPSS version 21.0. Because this study involved the analysis of routinely collected data at an aggregate level, ethics approval was not required or sought.
Results
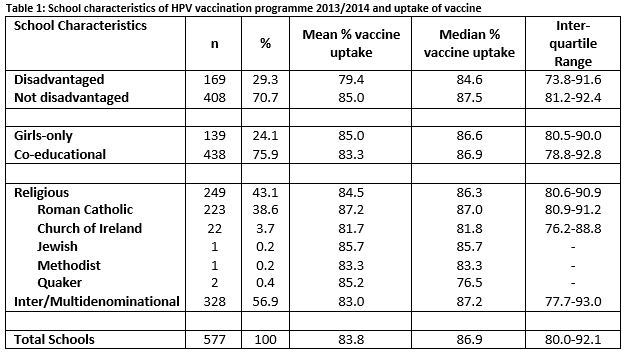
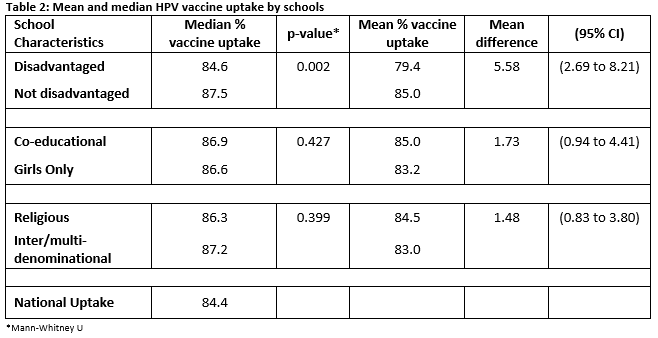
A total of 577 schools were identified with a cohort of 30,404 girls for vaccination for the 2013/2014 year. School characteristics and mean vaccine uptake are shown in Table 1. Mean national vaccine uptake was 83.8%, (IQR 80-92%). Univariate analysis, comparing mean and median vaccine uptake between schools with different characteristics, identified a lower mean and median vaccine uptake in disadvantaged schools (DEIS schools) compared with other schools (Table 1). Disadvantaged schools had a lower uptake of vaccine for 2nd and 3rd doses of vaccine (Table 4). Differences in uptake increased for each subsequent dose. Other school characteristics did not affect vaccine uptake (Table 4). Univariate analysis of mean and median (%) HPV vaccine uptake across schools of different religious ethoses revealed no statistically significant difference in uptake (%) (Wilcoxon rank sum test p=0.567).
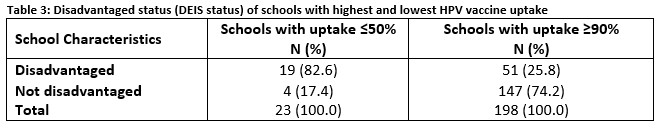
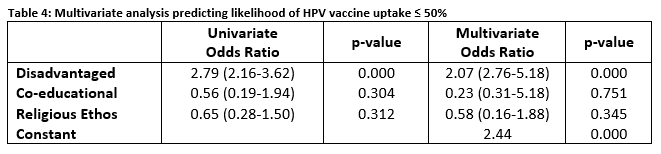
Analysis of schools with the lowest and highest uptake was undertaken. Of those schools with uptake ≤ 50%, 83% were disadvantaged schools (Table 2). Multivariate analysis was used to explore determinants of HPV vaccine uptake ≤50% in schools. Disadvantage made a statistically significant contribution to the model (Table 3).Disadvantaged schools were twice as likely to have a vaccine uptake ≤ 50% compared to other schools. Co-educational status and religious ethos did not contribute to the model.
Discussion
At the time of writing, HPV vaccine uptake in Ireland was high, and even in schools that are disadvantaged was above the national target of 80%. Since then, anti-HPV vaccine publicity as had a negative impact on national HPV vaccine uptake in Irish schools. Notwithstanding recent anti- HPV vaccine publicity, school based programmes, such as the Irish HPV vaccination programme have been shown to maximise uptake of vaccines when compared with opportunistic community based programmes12,13. However, our study demonstrates that inequity in uptake may persist in school based programmes. While the difference in mean and median uptake between disadvantaged schools and other schools in our study was small, the majority of schools with the lowest uptake (≤ 50%) were disadvantaged. Disadvantaged schools were twice as likely to have an uptake of ≤ 50% when compared with other schools, independent of other school characteristics. Lower HPV vaccine uptake in disadvantaged schools has been reported by other studies; in Manchester, uptake was significantly lower in more deprived areas5 while in Ontario, Canada, uptake of HPV vaccine in schools was lower in girls from lower income backgrounds8. Our study is however, limited by the fact that it was not possible to determine if any individual student characteristics affect uptake. Ethnicity could not be measured in our study which may be a factor4,16. Language and literacy difficulties may impact on parents’ ability to complete consent forms for vaccination, and therefore affect uptake as may other characteristics of students such as parental education.
The relationship between disadvantage and HPV vaccine uptake in schools is complex. Parents from disadvantaged backgrounds may be less likely to respond to offers of vaccination, while those from the most affluent areas are more likely to actively refuse vaccination 4. However, in some settings school vaccination programmes have been successful in minimising differences in uptake in disadvantaged groups. In the UK, uptake of HPV vaccine in girls in the target age-group for vaccination did not differ by small area deprivation score14. In New Zealand the school vaccination programme achieved the highest uptake in Maori and Pacific students who are traditionally disadvantaged. Uptake in the most disadvantaged schools was 93%2. Similarly, the Australian school HPV vaccination coverage achieved a relatively equal uptake across socio-economic groups15. In a study from the Southwest of England, HPV vaccine uptake in schools did not vary significantly by social deprivation5. Uptake may be affected by differences in which the school vaccination programme is delivered between countries. In England school nurses who have pre-existing links with schools deliver the school vaccination programme. They can identify girls likely to miss vaccines and engage with them and their parents8.
National vaccination policy is also an important factor. In New Zealand, achieving high coverage for Māori and Pacific girls are priorities of the National HPV Implementation Strategy. Specific HPV vaccine uptake targets are set and resources allocated16. Similarly in Scotland, the development of specific approaches to enhance equitable access to the vaccine were developed as part of their HPV vaccine programme which achieved over 90% uptake17. In Ireland, no specific programmes exist to target HPV vaccine in disadvantaged girls and no additional resources allocated. The vaccination programme is delivered by teams who do not have a pre-established relationship with schools and no way of identifying disadvantaged students. Data protection legislation means that vaccination teams are not given the names and contact details of students to be vaccinated in each school. Rather, they receive a total number of students for vaccination. Teachers are responsible for distributing vaccination information and consent forms to students who give this information to their parents. If parents refuse vaccination, they are asked to return the completed consent form, stating their refusal of vaccination, to vaccination teams. However if consent forms are not returned, in the absence of the names and contact details of the girls for vaccination, follow-up of non-responders is difficult if not impossible. Furthermore, registries with the names and contact details of girls eligible for HPV vaccination, allowing for call and recall do not exist. Call and recall systems for vaccination has been shown to be effective in improving vaccination rates18.
Our study shows that the difference in uptake between disadvantaged schools and other schools increased for each subsequent dose of HPV vaccine (Supplementary Table 1); the inability to call and recall students for vaccination may have had an impact on this. The question remains as to how HPV vaccine uptake can be improved in disadvantaged schools. Actively encouraging vaccination in students from disadvantaged schools requires closer relationships with schools than currently exists. Engaging with education authorities has had a positive impact on HPV programmes in other countries17, 19. The identification of individual students who have not been vaccinated and their follow-up requires a change in data protection legislation and the development of health information systems and vaccination registries. Our study was undertaken before anti-HPV vaccine publicity negatively affected uptake rates of HPV vaccine in Ireland. The impact of anti-vaccine publicity on HPV uptake requires careful ongoing monitoring particularly in disadvantaged schools to determine if the decline in uptake has disproportionately affected disadvantaged schools. Further research is needed regarding factors that affect uptake of HPV vaccine both at a school level and at an individual student level. Policy makers and vaccination teams should develop specific strategies targeted at disadvantaged schools in order to ensure a more equitable uptake of HPV vaccine. The importance of developing vaccination policy that targets disadvantaged groups has been effective in other countries. Achieving equitable HPV vaccine uptake is vital if inequalities in cervical cancer morbidity and mortality are to be addressed.
Correspondence:
Dr Chantal Migone, Department of Public Health, HSE Area East, Dr Steevens’ Hospital, Dublin 8
Email: [email protected]
Conflict of Interest:
The authors declare no conflict of interests
References
1. Leval A, Herweijer E, Ploner A, Eloranta S, Fridman Simard J, Dillner J, Young C, Netterlid E, Sparen P, Arnheim-Dahlstrom L. Quadrivalent human papillomavirus vaccine effectiveness: a Swedish national cohort study. J Natl Cancer Inst. 2013;105(7):469-74.
2. Poole T, Goodyear-Smith F, Petousis-Harris H, Desmond N, Exeter D, Pointon L, Jayasinha R. Human papillomavirus vaccination in Auckland: reducing ethnic and socioeconomic inequities. Vaccine. 2012;31(1):84-8.
3. Hofstetter AM, Rosenthal SL. Factors impacting HPV vaccination: lessons for health care professionals. Expert Rev Vaccines. 2014;13(8):1013-26.
4. Roberts SA, Brabin L, Stretch R, Baxter D, Elton P, Kitchener H, Mc Cann R. Human papillomavirus vaccination and social inequality: results from a prospective cohort study. Epidemiol Infect. 2011;139(3):400-5.
5. Fisher H, Audrey S, Mytton JA, Hickman M, Trotter C. Examining inequalities in the uptake of the school-based HPV vaccination programme in England: a retrospective cohort study. J Public Health (Oxf). 2014;36(1):36-45.
6. Ogilvie G, Anderson M, Marra F, McNeil S, Pielak K, Dawar M, Mc Ivor M, Ehlen T, Dobson S, Money D, Patrick DM, Naus M. A population-based evaluation of a publicly funded, school-based HPV vaccine program in British Columbia, Canada: parental factors associated with HPV vaccine receipt. PLoS Med. 2010;7(5):e1000270.
7. Smith LM, Brassard P, Kwong JC, Deeks SL, Ellis AK, Levesque LE. Factors associated with initiation and completion of the quadrivalent human papillomavirus vaccine series in an Ontario cohort of grade 8 girls. BMC Public Health. 2011;11:645.
8. Fisher H, Trotter CL, Audrey S, MacDonald-Wallis K, Hickman M. Inequalities in the uptake of human papillomavirus vaccination: a systematic review and meta-analysis. Int J Epidemiol. 2013;42(3):896-908.
9. Sinka K, Kavanagh K, Gordon R, Love J, Potts A, Donaghy M, Roberstson C. Achieving high and equitable coverage of adolescent HPV vaccine in Scotland. Journal of epidemiology and community health. 2014;68(1):57-63.
10. Health Protection Surveillance Centre. Immunisation Uptake Statistics 2016 [Available from: http://www.hpsc.ie/A-Z/VaccinePreventable/Vaccination/ImmunisationUptakeStatistics/.
11. Department of Education and Skills. DEIS: delivering Equality of Opportunity in Schools [Available from: http://www.education.ie/en/Schools-Colleges/Services/DEIS-Delivering-Equality-of- Opportunity-in-Schools-/.
12. Kessels SJ, Marshall HS, Watson M, Braunack-Mayer AJ, Reuzel R, Tooher RL. Factors associated with HPV vaccine uptake in teenage girls: a systematic review. Vaccine.
2012;30(24):3546-56.
13. Gallagher KE, Kadokura E, Eckert LO, Miyake S, Mounier-Jack S, Aldea M, Ross DA, Watson-Jones D. Factors influencing completion of multi-dose vaccine schedules in adolescents: a systematic review. BMC Public Health. 2016;16:172.
14. Hughes A, Mesher D, White J, Soldan K. Coverage of the English national human papillomavirus (HPV) immunisation programme among 12 to 17 year-old females by area-level deprivation score, England, 2008 to 2011. Euro Surveill. 2014;19(2).
15. Barbaro B, Brotherton JM. Assessing HPV vaccine coverage in Australia by geography and socioeconomic status: are we protecting those most at risk? Aust N Z J Public Health. 2014;38(5):419-23.
16. HPV Project Team, Population Health, Directorate Ministry of Health. The HPV Immunisation Programme: National Implementation Strategic Overview. New Zealand 2008.
17. Potts A, Sinka K, Love J, Gordon R, McLean S, Malcolm W, Ross D, Donaghy M. High uptake of HPV immunisation in Scotland--perspectives on maximising uptake. Euro Surveill. 2013;18(39).
18. Jacobson Vann JC, Szilagyi P. Patient reminder and patient recall systems to improve immunization rates. Cochrane Database Syst Rev. 2005(3):Cd003941.
(P603)