Vaccine-Preventable Admissions to an Irish Paediatric Intensive Care
Y Doyle1, M Healy1,2, C McMahon 1,2, S Crowe 1,2
1Paediatric Intensive Care Unit, Our Lady’s Children’s Hospital, Crumlin, Dublin 12.
2University of Dublin, Trinity College, Dublin 2.
Abstract
In the Republic of Ireland, the schedule of state-funded immunisation for children is comprehensive and includes diphtheria, pertussis, tetanus, pneumococcus, hepatitis B, meningococcus C, haemophilus B, polio, measles, rubella and mumps. Varicella and meningococcal B vaccines are commercially available but are not currently funded by the government. Each of the illnesses preventable by these vaccines can cause substantial morbidity, and rarely mortality, in infants and children. Our PICU continues to see serious illness due to avoidable infection. There were 39 admissions in a 4 year period, with 34 children surviving to discharge. Nine children were infected with pneumococcus, with 4 deaths. There was one case of pertussis, causing death. Most infections occurred in previously healthy children. These preventable conditions represent a significant burden on children, families, and on social and healthcare resources.
Introduction
Children who do not receive immunisation remain vulnerable to life-threatening infection from a number of different bacterial and viral pathogens. In Ireland, children are offered vaccination as part of the State-funded scheduled immunisation programme1. There are several additional vaccines available through general practitioners (GP), with parents paying for the vaccine and its administration.
Each year, the 23-bed university-affiliated Paediatric Intensive Care Unit in Our Lady’s Children’s Hospital, Crumlin, admits 900-1100 patients. This paper describes the ongoing pattern of admission and outcomes due to vaccine preventable conditions over a four year period. This pattern may change in the future, as vaccines are added to the funded schedule.
Methods
This study was a retrospective review of admission data from 2011-2015 using existing data collection and recording tools (PicaNet and ICIP). Ethics committee approval was waived as it is part of ongoing clinical data collection. All children admitted to PICU with a diagnosis of sepsis secondary to a bacteria or virus for which there is a widely available vaccine were included.
Results
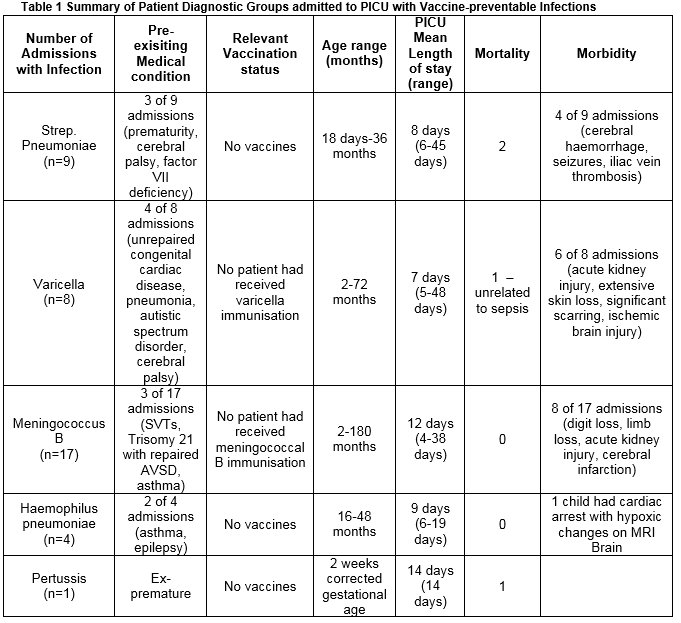
There were 39 admissions, (3.7% of total PICU admissions), with 34 children surviving to discharge (Table 1). There were no admissions with hepatitis B, diphtheria, measles, mumps, rubella, polio and meningococcal C infections. Streptococcus pneumoniae infection accounted for 9 admissions, meningococcus B infection precipitated 17 admissions, varicella 8 admissions, haemophilus influenza 4 admissions, and there was one admission due to pertussis infection. Death occurred in four children infected with pneumococcus, and one infant with pertussis. There were no deaths in the varicella or meningococcal patients. Serious morbidity occurred in 19 of 39 admissions, and varied from skin loss requiring grafting, limb and digit loss, seizures, acute kidney injury and haemorrhagic cerebral infarction.
Discussion
There are many reasons why children do not receive their scheduled immunisation, including illness2. Children are screened for fever, rash and malaise before vaccination, and this may result in planned vaccination being deferred. Parents may choose not to have their child immunised following the routine schedule because of concerns over the effects of vaccine medications2,3. There were no cases of vaccine failure resulting in serious illness. Eight younger infants who presented with severe pneumococcal infection less than 6 weeks of age had not commenced their schedule of vaccines. One infant was admitted to PICU with pertussis infection, at corrected age of two weeks. The infection occurred 4 weeks before the anticipated age for administration, and this child did not survive. Neonates rely on herd immunity to protect them against infection4,5. The level of immunity decreases when overall rates of immunisation fall within a community6, which is why the Health Protection Surveilance Centre (HPSC) has strongly recommended that pregnant women receive pertussis immunisation in the third trimester7. Children with varicella infection (n=8), presented with secondary bacterial infection. Organisms isolated included invasive Group A Streptococcus and Staphylococcus aureus, and these super-infections led to systemic sepsis, cellulitis and empyema. Varicella infection may be avoided with an organism-specific vaccine, which is not funded by the Irish Health Service8. Parents may ask their GP to administer this two-dose vaccine at an average cost of €300.
Meningococcal B sepsis was the largest diagnostic group (n=17), with 10 patients experiencing serious morbidity. There were no deaths in this group, reflecting improvements in early recognition and critical care management9. The vaccine for meningococcal B infection is commercially available since 2014, at a cost of approximately €300. Routine administration as part of the primary schedule is planned. Families who cannot afford to pay would not be offered these vaccines routinely. Our audit illustrates that bacterial and viral infection continues to result in significant morbidity and mortality in a small number of Irish children. Most of these infections and their subsequent burden of illness may be avoided with immunisation. Critical care admission is costly in terms of physical, psychological and family support required, and in socio-economic terms10. Although overall numbers are small, each case represents a child and family who have had a traumatic and avoidable experience, some with serious longterm consequences.
Correspondence:
Suzanne Crowe MB FFARCSI FJFICM
Paediatric Intensive Care Unit, Our Lady’s Children’s Hospital, Crumlin, Dublin 12., University of Dublin, Trinity College, Dublin 2.
Email: [email protected]
Telephone: 014096000
Conflicts of interest:
There were no external or internal sources of funding sought or obtained in preparation of this paper. The authors do not have any conflict of interest in issues discussed in this manuscript.
References
1. Primary Immunisation Schedule. www.hse.ie/immunisation/publicinformation/PrimaryImmunisationSchedule. Accessed July 1st 2016.
2. Pearce A, Marshall H, Bedford H. Barrier to childhood immunisation: Findings from the Longitudinal Study of Australian Children. Vaccine 2015 Jun 26;33:3377-83. Epub 2015 May 21.
3. McKee C, Bohannon K. Exploring the Reasons behind Parental Refusal of Vaccines. J Pediatr Pharmacol Ther 2016 Mar-Apr;21:104-9
4. Haddy R, Perry K, Chacko CE, Helton WB, Bowling MG, Looney SW, Buck GE. Comparison of incidence of invasive Streptococcus pneumoniae disease among children before and after introduction of conjugated pneumococcal vaccine. Pediatr Infect Dis J 2005 Apr;24:320-3
5. Waye A, Jacobs P, Tan B. The impact of the universal infant varicella immunisation strategy on Canadian varicela-related hospitalisation rates. Vaccine 2013 Oct 1;31:4744-8. Epub 2013 Aug 20.
6. Martin Ng, Sadarangani M, Pollard AJ, Goldacre MJ. Hospital admission rates for meningitis and septicaemia caused by Haemophilus influenzae, Neisseria meningitidis, and Streptococcus pneumoniae in children in England over five decades: a population-based observational study. Lancet Infect Dis 2014 May;14:397-405. Epub 2014 Mar 14
7. Guidelines for the Public Health Management of Pertussis. Health Protection Surveilance Centre, Deaprtment of Health 2013. http://www.hpsc.ie/…/VaccinePreventabe/PertussisWhoopingCough.pdf. Accessed October 28th 2016
8. Marin M, Marti M, Kambhampati A, Jeram SM, Seward JF. Global Varicella Vaccine Effectiveness: A meta-analysis. Pediatrics 2016 Mar;137:e20153741. Epub 2016 Feb 16.
9. Akcan Arikan A, Williams EA, Graf JM, Kennedy CE, Patel B, Cruz AT. Resuscitation Bundle in Pediatric Shock Decreases Acute Kidney Injury and Improves Outcomes. J Pediatr 2015 Dec;167:1301-5.e1. Epub 2015 Sep 26.
10. Aspesberro F, Mangione-Smith R, Zimmerman JJ. Health-related quality of life following pediatric critical illness. Intensive Care Med 2015 Jul;41:1235-46.
(P560)